New findings offer hope towards novel tailored immunotherapies against brain tumours
Luxembourg Institute of Health unveils how brain cancer hijacks immune cells to its advantage
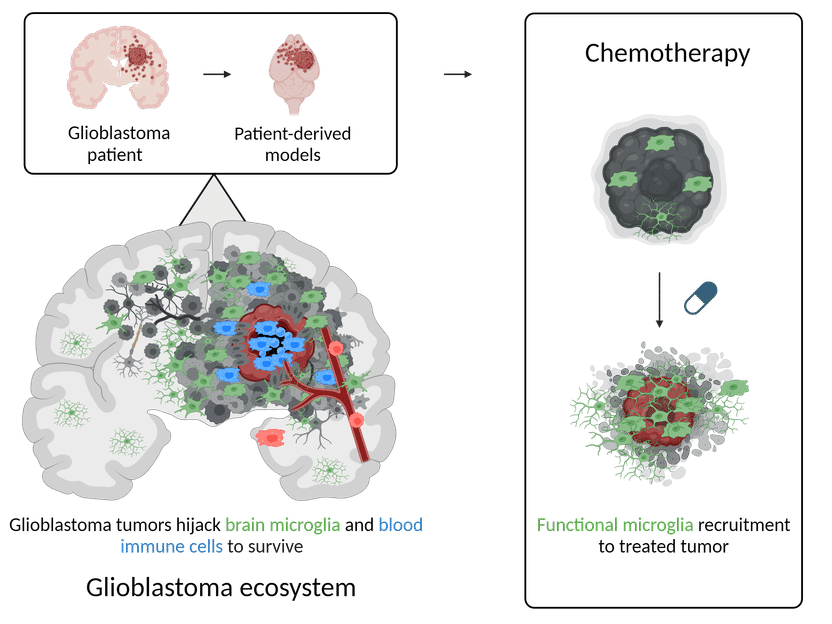
A comprehensive study led by Luxembourg Institute of Health (LIH) Dr Anna Golebiewska, Group Leader at the NORLUX Neuro-Oncology Laboratory, and Dr Alessandro Michelucci, Group leader of the Neuro-Immunology Group, shed light on the intricate interplay between glioblastoma (GBM) tumours and the immune system within the brain. Published in a recent issue of Genome Medicine, the research provides crucial insights into the diversity of the GBM ecosystem and its plastic response to treatment, offering potential avenues for future immunotherapeutic strategies.
Luxembourg Institute of Health
GBM, the most aggressive form of primary brain tumour, poses significant challenges due to its ability to hide from and evade the immune system. The study delves into the tumour microenvironment, specifically focusing on the role of myeloid cells, a type of immune cell, in supporting tumour growth and escape from chemotherapeutic treatments.
The collaborative efforts between different groups of the LIH Department of Cancer Research, together with partners at the Luxembourg Centre for Systems Biomedicine at the University of Luxembourg, the Laboratoire National de Santé, Centre Hospitalier de Luxembourg and the University of Freiburg, enabled the scientists to combine advanced techniques such as single-cell RNA sequencing, spatial transcriptomics, and functional assays, to examine both patient tumours and patient-derived orthotopic xenografts (small replicas of patient tumours that are grown in the lab). Together, they discovered that GBM tumour cells intricately instruct their neighbouring microenvironment to survive and evade the immune system.
Of particular significance was the discovery of the diverse characteristics of microglia, a unique type of immune cell residing in the brain, in response to signals received from GBM. Indeed, it appears that in contact with GBM these microglia change their appearance and behaviour, to mimic both phagocytic cells (responsible for engulfing and destroying harmful substances) and dendritic cells (involved in educating other immune cells from the blood). Additionally, the research shed light on how treatment with temozolomide, a standard-of-care chemotherapy, alters the molecular makeup of both the tumour and its surrounding microenvironment. This finding underscores the importance of understanding the complex interactions within the brain tumour ecosystem for devising effective treatment strategies.
Dr Golebiewska emphasized the significance of the study’s findings, stating, “Our research provides crucial insights into the adaptive nature of the GBM ecosystem and its implications for treatment strategies. By unravelling the complexities of the tumour microenvironment, we aim to pave the way for more effective immunotherapies tailored to combat GBM.“
The study emphasises the importance of advances patient-derived models in mirroring key aspects of the complex GBM ecosystem, providing valuable insights into treatment responses and resistance mechanisms. The integration of high-quality patient cohorts, preclinical models, multiomics data, and advanced bioinformatics represents a significant step forward in cancer research.
"This groundbreaking study not only advances our understanding of GBM biology but also holds promise for the development of novel immunotherapeutic approaches aimed at targeting the complex interactions within the tumour microenvironment," concludes Dr Michelucci.