Hijacking in the immune system
The human cytomegalovirus reprograms cellular defence mechanisms
The human cytomegalovirus, HCMV for short, lies dormant unnoticed in the body of most people for their entire lives. In immunocompromised individuals, however, the virus can cause life-threatening infections. It infects dendritic cells, a specific type of cell in the immune system. Although the majority of them are infected, only a few of them immediately execute the virus's genetic programme. Researchers at TWINCORE, Centre for Experimental and Clinical Infection Research, have now been able to show which signalling pathways of the innate immune system the virus is targeting in order to have itself produced by the host cells. They have published their findings in the journal Nature Communications.
Dr. Bibiana Costa, first author of the study, in the lab.
©TWINCORE/Grabowski
Up to 90% of the world's population carries HCMV. In people with a normal immune system, the infection is usually subclinical, i.e. it does not cause any pronounced symptoms. However, in immunocompromised patients, such as organ transplant recipients, the infection can become life-threatening. In addition, infection with HCMV during pregnancy is the most common cause of malformations in newborns, such as congenital hearing impairment.
In the human body, HCMV can infect the myeloid cells of the immune system. This group also includes the dendritic cells derived from monocytes, whose main task is to process foreign proteins so that they can be presented to the T cells. Antigen-specific T cells can then eliminate infected cells.
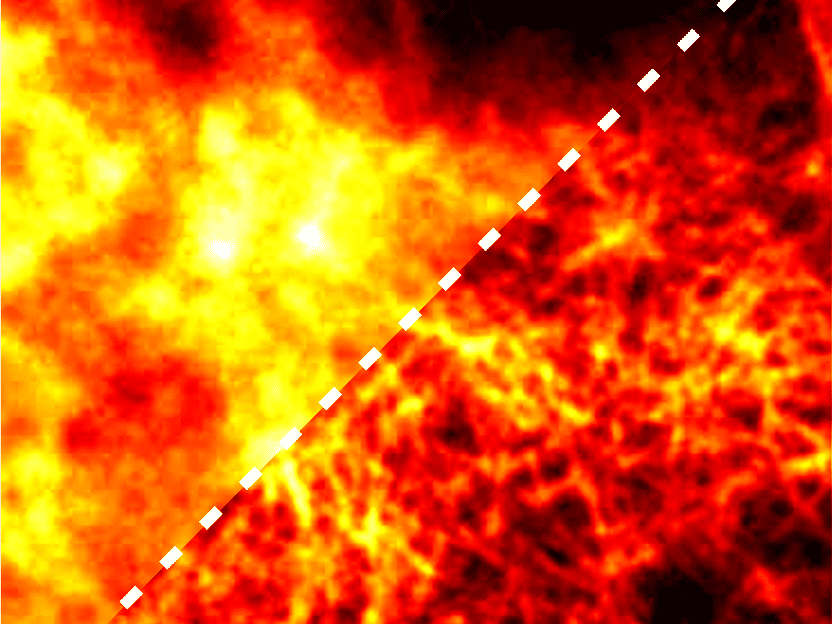
The researchers from the Institute for Experimental Infection Research, led by Prof Ulrich Kalinke, were able to divide the monocyte-derived dendritic cells into three groups, one of which is more susceptible to infection than the others. "Using single-cell RNA sequencing, we found that in these cells the signalling pathway that normally recognises viruses is virtually hijacked by HCMV in order to establish the productive infection," says Dr Bibiana Costa, postdoctoral researcher at TWINCORE and first author of the study. "This is the so-called STING signalling pathway." STING stands for "stimulator of interferon genes".
Interferons are messenger substances of the immune system that act directly against viruses and can also activate defence cells. In addition, interferons trigger further defence processes in a chain reaction. In the subgroup of dendritic cells, which are particularly susceptible to infection, the virus' own proteins block this protective function and instead reprogramme them so that new virus particles are produced undisturbed.
"We then analysed this viral intervention in the cellular process in more detail to find out exactly which genes in the cells are affected," says Costa. "We were able to identify several candidates that have either antiviral or proviral properties." Because certain immunomodulating drugs intervene precisely in these signalling pathways, there may be potential here for a therapeutic approach. This seems particularly promising because organ transplant recipients have to take immunosuppressive drugs for the rest of their lives to prevent the immune system from rejecting the transplant. "However, this requires further studies," says Prof Ulrich Kalinke, Director of the Institute for Experimental Infection Research and Managing Director of TWINCORE.
In addition to the researchers from TWINCORE, cooperation partners from several research institutions were involved in the study, including the Helmholtz Institute for RNA-based Infection Research HIRI in Würzburg, the University of Regensburg, the Helmholtz Centre for Infection Research in Braunschweig and the Hannover Medical School. "The RESIST Cluster of Excellence also supports us in networking," says Kalinke. "Without these partnerships, we would not be able to conduct translational infection research at a high level."
Original publication
Bibiana Costa, Jennifer Becker, Tobias Krammer, Felix Mulenge, Verónica Durán, Andreas Pavlou, Olivia Luise Gern, Xiaojing Chu, Yang Li, Luka Čičin-Šain, Britta Eiz-Vesper, Martin Messerle, Lars Dölken, Antoine-Emmanuel Saliba, Florian Erhard, Ulrich Kalinke; "Human cytomegalovirus exploits STING signaling and counteracts IFN/ISG induction to facilitate infection of dendritic cells"; Nature Communications, Volume 15, 2024-2-26