How stem cells and immune cells communicate
Lisec Artz Award for Simon Haas: Groundbreaking discovery of an unknown protective mechanism against blood cancer from stem cells
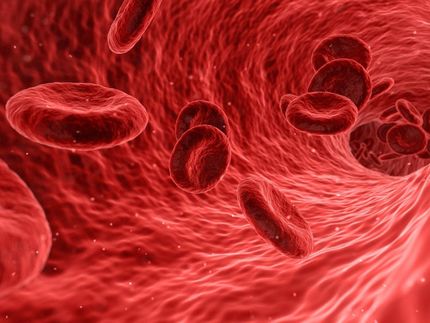
blood cancer is often driven by mutations in stem cells, which are key target cells in the search for innovative early-stage therapies. Dr. Simon Haas, head of a lab within the joint research focus of the Berlin Institute of Health at Charité (BIH), Charité – Universitätsmedizin Berlin, and the Max Delbrück Center, is seeking to understand interactions between stem cells and immune cells. In a groundbreaking discovery, he found a previously unknown protective mechanism that prevents blood cancer from developing from stem cells.

Dr. Simon Haas
Felix Petermann, Max Delbrück Center
For this and other scientific contributions, Haas has now been awarded the Lisec-Artz Prize, endowed with €10,000, which the University of Bonn Foundation gives each year to an outstanding early-career cancer researcher.
“Stem cells are very fascinating, but our knowledge of these indefinitely dividing cells is still incomplete,” explains Dr. Simon Haas. “We expect further research into stem cells will give an important boost to the development of therapies that would allow us to intervene early on in the pathological processes of blood cancers.” After stints at the German Cancer Research Center (DKFZ) in Heidelberg and at the Massachusetts Institute of Technology (MIT) and Harvard University in Boston, USA, Haas moved to Berlin in 2020 to lead a research group within the joint research focus “Single Cell Approaches for Personalized Medicine” of the Berlin Institute of Health at Charité (BIH), the Max Delbrück Center, and Charité – Universitätsmedizin Berlin.
Listening in on cell-to-cell chatter
Haas and his team are “communication researchers”: They are interested in decoding the crosstalk between stem cells and immune cells. There are high hopes in the hemato-oncology field that novel immunotherapies will more effectively harness the body’s immune system to fight cancer cells. But developing such therapies requires a precise understanding of the communication between cancer cells and immune cells. If T cells recognize that cells have mutated based on certain signals, they can trigger their elimination. Yet early elimination often fails because cancer cells suppress the telltale signals or manipulate the immune cells using other deceptive tricks.
Haas has big plans to “listen in” and decipher the communication between stem cells and immune cells. An important step toward this goal was the discovery that stem cells express so-called MHC-II molecules on their surface and use them to communicate with specific T cells, the T helper cells. This was a huge surprise for Haas, because it was at variance with the then accepted theory that only certain immune cells, such as macrophages and B cells, could present antigens with the help of MHC-II molecules in order to initiate defense mechanisms against viruses or bacteria.
Since stem cells, which constantly replenish the supply of fresh blood cells in a process known as hematopoiesis, divide indefinitely, there is a real risk that cells will mutate and spread during this process. So it makes sense for T-cells to be present in order to immediately eliminate suspicious cells that may become cancerous. Though not infallible, this protective mechanism is highly effective due to the fact that mutated stem cells communicate directly with T cells and signal that something is wrong without having to involve other immune cells for the purpose of antigen presentation. The interaction with the T cells leads to the mutated stem cells being rapidly removed from the system, thereby warding off the potential risk of developing blood cancer.
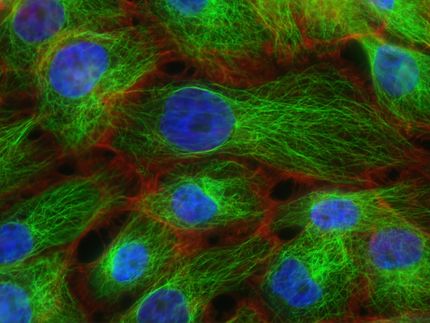
The researchers are monitoring cell-to-cell crosstalk using single-cell analysis, a technique which Haas wants to develop further for his own research purposes. He and his team are based at the Berlin Institute for Medical Systems Biology of the Max Delbrück Center (MDC-BIMSB), which provides an excellent technological infrastructure for this work. “Using this innovative method, we aim to identify the relevant signals by investigating millions of cell pairs from individual stem and immune cells that are communicating with each other,” says Haas. “We are interested in such things as: Which signals cause a mutated cell to be eliminated? Which signals block the immune cells from attacking? Temporal processes play a key role when it comes to therapeutic interventions, so we also aim to find out which type of interaction takes place and in which stage of the disease.”
Chance for a cure?
If researchers knew what strategies mutated cells use to evade T-cell attack, they could selectively target them and thwart the cunning tricks of cancer cells. The aim is to intervene early on in the process of leukemia development, which would significantly increase the chances of curing patients. “Ideally,” says Haas, “we will eventually be able to stop the pathological process even before blood cancer occurs.” The research group is currently developing precision diagnostics and prognostics that enable early disease detection and personalized treatment strategies.
Other news from the department science
Most read news
More news from our other portals
See the theme worlds for related content
Topic World Cell Analysis
Cell analyse advanced method allows us to explore and understand cells in their many facets. From single cell analysis to flow cytometry and imaging technology, cell analysis provides us with valuable insights into the structure, function and interaction of cells. Whether in medicine, biological research or pharmacology, cell analysis is revolutionizing our understanding of disease, development and treatment options.
Topic World Cell Analysis
Cell analyse advanced method allows us to explore and understand cells in their many facets. From single cell analysis to flow cytometry and imaging technology, cell analysis provides us with valuable insights into the structure, function and interaction of cells. Whether in medicine, biological research or pharmacology, cell analysis is revolutionizing our understanding of disease, development and treatment options.