Genetically engineered stem cells to boost cancer immunotherapy
Researchers sign an agreement to research the production of CAR-NK cells, which are easier to produce than CAR-T cells used successfully in immunotherapy
Advertisement
CSIC, the Banc de Sang i Teixits (BST) de Catalunya and the Institut d'Investigació Biomèdica de Bellvitge (Idibell) have signed an agreement to investigate the genetic modification of stem cells obtained from umbilical cord blood to produce CAR-NK immune cells capable of recognizing and attacking tumor cells and other diseases.
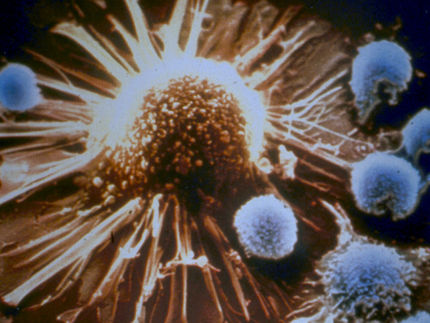
The research aims to improve the results of CAR-T (chimeric antigen receptor T-cell) therapies, which are already in use for some types of cancer. The main difference is that NK (Natural Killer) cells are easier to produce on a large scale from stem cells than T cells.
The agreement aims to create a bank of CAR-NK cells containing a battery of antitumor genes, including CAR19 or CAR19/20 receptors. The latter are genetic modifications that enable immune cells to specifically identify and attack acute lymphoblastic leukemia and B-cell lymphoma. The aim is to store these cells in cell banks and have them available for immediate application in immunotherapy treatments against cancer.
To this end, the CSIC will make available to the project the two patented technologies developed at the Margarita Salas Biological Research Center (CIB-CSIC) in Madrid by the team led by researcher Daniel Bachiller, which make it possible to introduce genetic modification into immune cells to make them capable of recognizing and attacking tumor cells.
"We believe that our development will make it possible to produce immune system cells designed to attack specific therapeutic targets in a much faster, more effective and cheaper way than the technologies currently being tested. Our system can also be applied to other diseases, such as fungal infections or those caused by antibiotic-resistant bacteria," explains Daniel Bachiller of the CIB.
For its part, the BST will provide the induced pluripotent stem cells from umbilical cord blood and will produce the NK cells from them, and IDIBELL, whose research group is also attached to the Catalan Institute of Oncology (ICO), will provide the models for the in vitro and in vivo validation of the new therapies.
Exploratory research
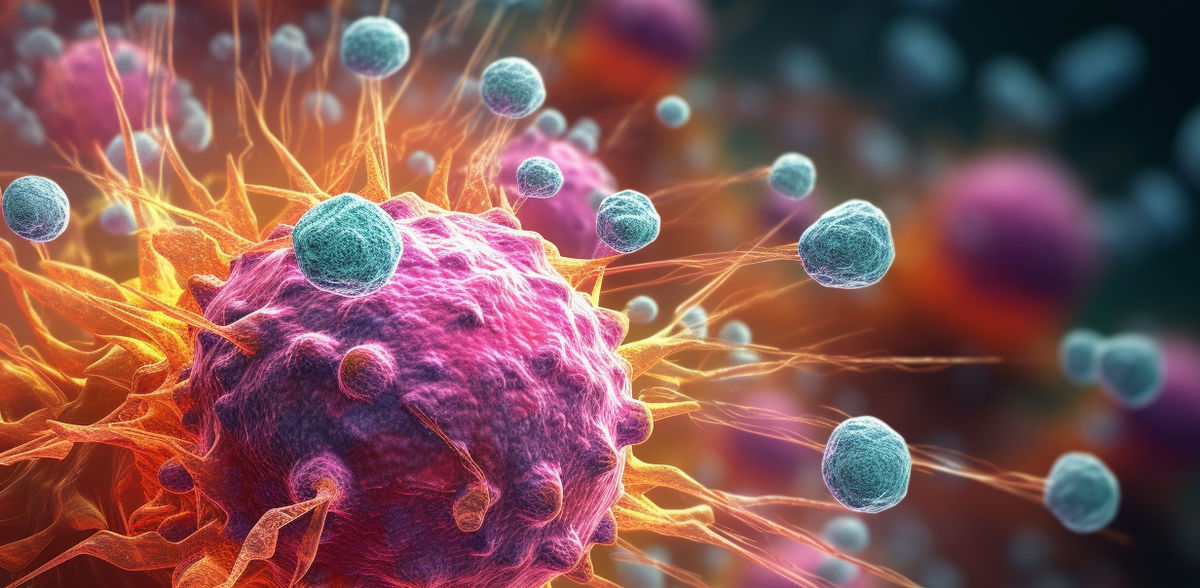
CAR-NK therapies (acronym for chimeric antigen receptor-mediated NK cells) are a promising strategy to combat cancer, still under development. They are based on modifying NK cells (natural killer cells, a type of lymphocyte) so that they are capable of recognizing and specifically attacking cancer cells.
The CSIC, BST and IDIBELL research, of a preliminary and exploratory nature, aims to obtain and modify these cells from umbilical cord stem cells, and then test their viability and effectiveness in the laboratory.
The stem cells used in this project, and therefore the NK cells derived from them, are from donors compatible with a high percentage of the European population. As a result, the cells can be produced and stored while awaiting the patients who need them.
At present, the patient's own lymphocytes are used, which have to be extracted, modified and cultured individually and after diagnosis, "which makes the procedure extraordinarily expensive and dangerously delays its application," explains Bachiller.
The research aims to confirm whether it is possible to improve the efficacy of current cellular immunotherapy treatments by endowing immunocompatible NK cells with a battery of antitumor genes that multiply the effect of CARs.
It is envisaged that the resulting cell bank, which will be at the BST, will contain modified cell lines of the most common genetic types. This would provide an immediately available CAR-NK cell bank for the treatment of acute lymphoblastic leukemia and B-cell lymphoma.
Note: This article has been translated using a computer system without human intervention. LUMITOS offers these automatic translations to present a wider range of current news. Since this article has been translated with automatic translation, it is possible that it contains errors in vocabulary, syntax or grammar. The original article in Spanish can be found here.