The harmful effects of immune cells in hypertension
“Our findings suggest that macrophages and microglia undergo extensive reprogramming during hypertension”
Advertisement
hypertension can damage the heart, brain, and blood vessels. The immune system plays an important role in this process, Suphansa Sawamiphak from the Max Delbrück Center reports in Cardiovascular Research. The study, using zebrafish, found that inflammation causes macrophages to damage blood vessels instead of protecting them.
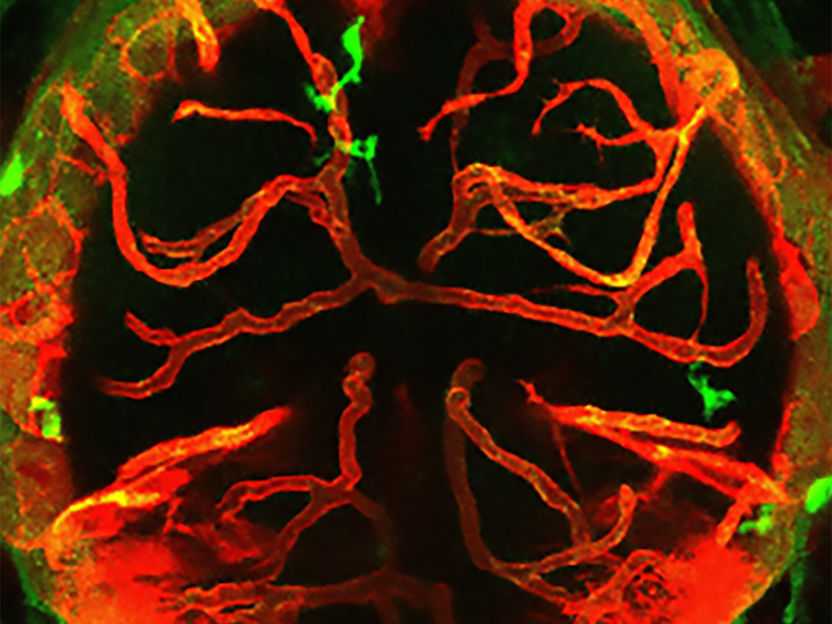
Interactions between macrophages/microglia and cerebral vessels lead to vascular regression and cell death in the brain. Image depicting the brain of a zebrafish with macrophages/microglia labeled in green and blood vessels in red.
Maria P. Kotini, University of Basel
Hypertension, or high blood pressure, tops the list of chronic health conditions. It affects about one-third of the world’s population, including nearly 44 percent of German citizens. If the pressure in the blood vessels is too high, the body’s organs – mainly the brain, the heart, and the blood vessels – suffer as a result. The consequences go beyond an increased risk of developing serious cardiovascular diseases like strokes or heart attacks. In a healthy body, the heart, brain, and blood vessels also play a key role in regulating blood pressure. If they are damaged by persistently high blood pressure, this regulatory ability is lost – creating a vicious circle.
To lower blood pressure, patients should make changes to their lifestyle, such as eating a well-balanced, low-salt diet, exercising regularly, and stopping smoking. Some drugs, like beta blockers and ACE inhibitors, can also help: “Conventional medications can lower blood pressure, but they fail to achieve the desired protective effect on the organs in a large portion of patients,” says Dr. Suphansa Sawamiphak, who heads the Cardiovascular-Hematopoietic Interaction Lab at the Max Delbrück Center. This is particularly evident, she says, in the brain, where hypertension causes tiny blood vessels to become permeable, or eventually die off, adding: “This means there must be other control centers in the overall process that we can’t target with conventional therapeutic agents.”
Researchers have known for some time that components of the immune system may play a role here. Inflammatory responses in the body contribute to high blood pressure and have harmful effects on organs, but it is not yet known exactly how this occurs.
Immune cells damage blood vessels in the zebrafish brain
So Sawamiphak and her team at the Max Delbrück Center and collaborators working in Italy and Switzerland, studied larval zebrafish to shed more light on the underlying biological mechanisms. “This is an excellent model system for investigating many questions, since it is easy to manipulate the organisms by changing the environment,” explains the biologist, adding: “Because young zebrafish are transparent, we can literally see how this affects the living fish.”
To analyze the role of the immune system in hypertension, the research team raised zebrafish larvae in water with low ion concentration. This creates an ion imbalance in their bodies that is comparable to excessive salt consumption in humans, thus leading to high blood pressure. The team then examined how this affects the blood vessels in the brain.
According to the researchers’ observations, hypertension causes an increase in both the number of macrophages and microglia – special immune cells of the brain – that can get in touch with the vascular surface. There, they come into contact with the endothelium, the innermost cellular layer of blood vessels, and progressively weaken the vessel walls. Damage is also done to the blood-brain barrier, which prevents harmful substances and pathogens in the blood from reaching the brain. “The interesting thing is that when blood pressure levels are healthy, macrophages and microglia normally help protect the vessels,” says Sawamiphak. “Our findings suggest that macrophages and microglia undergo extensive reprogramming during hypertension.”
Blocking signaling molecules prevents organ damage
An important role is played by inflammatory messengers like interferon gamma, which are released at a higher rate under hypertensive conditions. To experimentally substantiate this connection, they switched off the gene for a receptor to which interferon gamma normally binds. In these fish, hypertension did not cause any damage to blood vessels or to the blood-brain barrier. The team also succeeded in demonstrating in mice that therapeutic agents that inhibit interferon gamma can prevent common side effects of hypertension – including damage to the blood-brain barrier, degradation of blood vessels in the brain, and cognitive deficits.
“Our findings provide a completely new perspective on the role of inflammatory processes in the progression of hypertension,” says Sawamiphak, explaining the significance of her work. Now, she says, it is necessary to more precisely characterize the immune cells and immunomodulators involved in such processes and to verify their role in higher animals including humans. If this can be confirmed, it would mean that the team had uncovered new therapeutic targets for hypertension through this study. This would particularly benefit patients for whom conventional drugs have failed to protect against progressive organ damage.