Long COVID study: blood values indicate reprogramming of immune cells
Clues for multiple subtypes of long COVID
Advertisement
The underlying mechanisms of long covid are not yet fully understood. Molecular clues to different subgroups of long COVID have now been provided by a research group at University Medicine Halle.
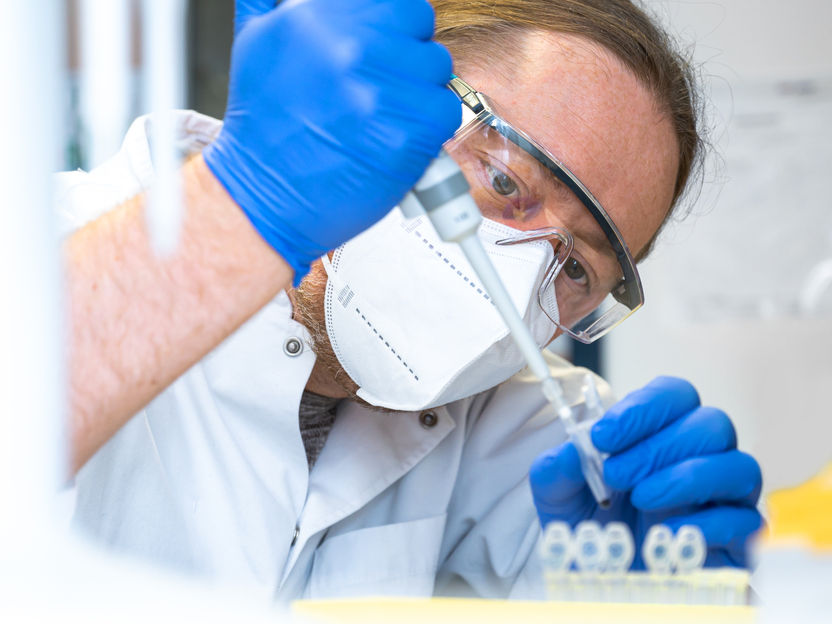
Dr. Christoph Schultheiss from University Medicine Halle profiling molecular blood levels.
University Medicine Halle
When symptoms persist: After recovering from a COVID-19 infection, many people suffer from a secondary disease called long COVID or post-COVID syndrome. A research group at University Medicine Halle has discovered molecular evidence for various long COVID subtypes. Patterns occur that could provide a potential therapeutic approach. The data suggest that various mechanisms lead to the development of the syndrome, including a “reprogramming” of immune cells. All of the participants were recruited through “DigiHero”, a Germany-wide study on digital health research conducted by University Medicine Halle. The results were recently published in the Journal of Medical Virology.
In the event of an infection, certain immune cells, called macrophages, make up the first line of defense in the body’s immune response. They, along with their precursors, monocytes, are important cells of the innate immune system. They play a crucial role in activating and regulating the immune response by secreting immunologic factors as signaling molecules. The research group from Halle, led by Professor Mascha Binder, has already shown that the concentration of three of these immunologic factors is elevated in the blood of people with long COVID symptoms. Until now, it was not clear to what extent the secretion of these factors was impaired and it was hypothesized that circulating viral remnants in the blood during the acute COVID-19 phase might influence the regulation of these immune cells.
Clues for multiple subtypes of long COVID
“Our study focused on other immunologic factors that promote inflammation and fibrosis which can be secreted by monocytes and macrophages,” explains Dr. Christoph Schultheiss, lead author of the study and research associate of the Department of Internal Medicine IV at University Medicine Halle. “It was shown that the release of these immunologic factors is significantly dysregulated in long COVID.” The scientists found that this “reprogramming” occurred in two distinct molecular patterns.
Additionally, blood levels of the viral S1 spike protein, which the COVID-19 virus uses to infect cells, were investigated. This protein was observed in some study participants following a COVID-19 infection, especially in those with long COVID. However, these blood values showed no correlation to the patterns of the dysregulated immune response, as previously assumed. “This was a relevant finding that we interpreted as indicative of distinct subgroups of long COVID that may result from divergent underlying mechanisms,” explains Schultheiß.
Individual symptoms do not allow conclusions to be drawn
It is also worth noting that the detected subtypes do appear to be independent to the symptoms of long COVID sufferers. “Clinically, long COVID is already well defined. Now we need to better understand the mechanisms involved in the development of the disease and link them to the clinical characteristics,” explains Professor Mascha Binder, head of the research group and director of the Department of Internal Medicine IV. “We were able to identify several immunologic factors in the blood and underscore the role they play in long COVID. Treatment options already exist for some of these factors in order to counteract this dysregulation,” says Binder.
Biospecimens obtained through Digital Health study
The published results also relied on the DigiHero study. DigiHero has already surveyed thousands of people across Germany about health-related issues via the digital platform. “We launched additional subprojects after the pandemic started. As a result, several hundred participants were recruited to answer questions about their history with COVID-19 and provide biospecimens of their blood for researchers to study,” reports Professor Rafael Mikolajczyk from the Institute for Medical Epidemiology, Biometrics and Informatics at University Medicine Halle.
Original publication
Schultheiß C, Willscher E, Paschold L, Gottschick C, Klee B, Bosurgi L, Dutzmann J, Sedding D, Frese T, Girndt M, Höll JI, Gekle M, Mikolajczyk R, Binder M. Liquid biomarkers of macrophage dysregulation and circulating spike protein illustrate the biological heterogeneity in patients with post-acute sequelae of COVID-19. J Med Virol. 2023 Jan;95(1):e28364

























































