Master hijackers: uncovering how leukaemia disarms the body’s defences
Microscopic vesicles released from leukaemia tumours and their surrounding cells prove critical in obstructing the body’s ability to fight cancer
Advertisement
A study led by the Tumor Stroma Interactions group at the Luxembourg Institute of Health has discovered that microscopic vesicles released by tumours and their surrounding cells in mice with chronic lymphocytic leukaemia hijack a specific branch of the body’s immune system and prevent it from destroying cancer cells. This finding, published in blood cancer Discovery, a journal of the American Association for Cancer Research, offers a crucial explanation for how cancers disarm the immune system and could provide a new avenue for the treatment of leukaemia and other cancers.
Symbolic image
Computer generated picture
Cancer is arguably the disease most likely to affect us, and one of the most difficult to cure or treat. One of the reasons of such resilience is that, unlike most other diseases, cancers can evade our immune system and even stop it working efficiently. This is particularly true for blood cancers, such as chronic lymphocytic leukaemia, which are highly immunosuppressive. How exactly do cancers switch off the body’s immune system? Like everything with cancer, the mechanism is multifaceted and researchers have been putting together the pieces of the puzzle for years.
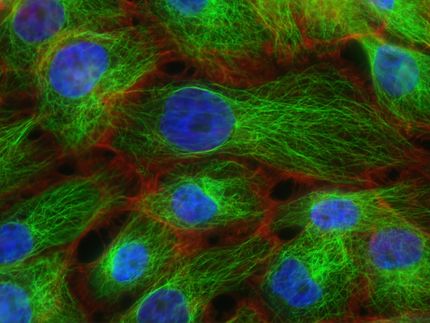
The Tumor Stroma Interactions (TSI) research group, led by Dr Jérôme Paggetti and Dr Etienne Moussay, at the Luxembourg Institute of Health (LIH) has now uncovered a key piece of this puzzle. They discovered that microscopic “sacs” called small extracellular vesicles (sEV for short) released in the tumour microenvironment (the region surrounding the tumour) of mice with chronic lymphocytic leukaemia (CLL) are directly responsible for dampening a specific component of the body’s immune system important for killing cancers, known as CD8+ T-lymphocytes.
Although we, and others, have previously shown a role for sEV in promoting CLL, the sEV used in those studies were mainly generated in a culture dish or ‘in vitro’, which might not fully reflect the situation in the living body. Now, scientists from the LIH Department of Cancer Research have isolated sEV directly from the tumour microenvironment in mice with CLL to examine how they promote cancer growth and progression.
"Within the tumour microenvironment, cancer cells are not the only cells that release sEV. What we isolated from the leukaemia microenvironment represent a cocktail of sEV that we’re likely to see in real life. Studying these sEV will provide important clues as to what’s really going on when leukaemia takes hold", explained Dr Paggetti, co-group leader of the TSI team and one of the lead investigators in this study.
The researchers found that these leukemic sEV have a distinct ‘fingerprint’ consisting of surface proteins and specific cargo material, which helps them suppress the immune response. They discovered that leukemic sEV are internalised by cells involved in the immune system. Moreover, the cargo carried by the leukemic sEV preferentially alter CD8+ T-cells rendering them ‘exhausted’ and unable to elicit an immune response. “This is different from what we saw using sEV generated in vitro before. sEV in the leukaemia microenvironment act as master hijackers that infiltrate immune cells and disarm them from within” emphasised Dr Moussay, co-group leader of the TSI team. In order to better understand the impact of sEV in vivo, the TSI team generated mice carrying a mutation preventing them from releasing sEV. The absence of sEV dramatic delay leukaemia development and progression in these mice. What’s more, typical leukaemia progression was restored when leukemic sEV were re-introduced in the same mice or when these mutated tumour cells were transferred to other mice lacking CD8+ T-cells.
"Our findings show unequivocally that the development and progression of chronic lymphocytic leukaemia depends on the interplay between sEV and CD8+ T-cells. This discovery has huge potential to change the course for future cancer treatments and the way we approach cancer research", summarised Dr Ernesto Gargiulo, lead author of the study.
The team also looked at whether leukemic sEV could serve as markers for disease outcomes in patients with CLL. They found that high expression of genes related to sEV biogenesis correlated with a more aggressive form of the disease, with poor prognosis and survival rates.
“The potential for sEV to also serve as markers for disease could lead to leukaemia patients being tested for sEV-related genes in the future in order to understand their prognosis and determine an appropriate treatment path,” concluded Dr Paggetti.