Same symptom – different cause?
Algorithms help to distinguish diseases at the molecular level
machine learning is playing an ever-increasing role in biomedical research. Scientists at the Technical University of Munich (TUM) have now developed a new method of using molecular data to extract subtypes of illnesses. In the future, this method can help to support the study of larger patient groups.

Head of the LipiTUM research group Dr. Josch Konstantin Pauling (left) and PhD student Nikolai Köhler (right) interpret the disease-related changes in lipid metabolism using a newly developed network.
LipiTUM
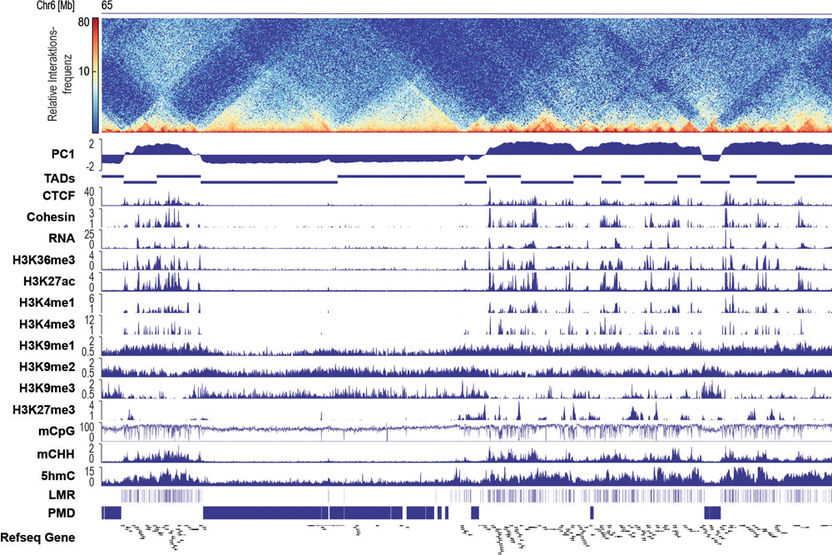
Nowadays doctors define and diagnose most diseases on the basis of symptoms. However, that does not necessarily mean that the illnesses of patients with similar symptoms will have identical causes or demonstrate the same molecular changes. In biomedicine, one often speaks of the molecular mechanisms of a disease. This refers to changes in the regulation of genes, proteins or metabolic pathways at the onset of illness. The goal of stratified medicine is to classify patients into various subtypes at the molecular level in order to provide more targeted treatments.
To extract disease subtypes from large pools of patient data, new machine learning algorithms can help. They are designed to independently recognize patterns and correlations in extensive clinical measurements. The LipiTUM junior research group, headed by Dr. Josch Konstantin Pauling of the Chair for Experimental Bioinformatics has developed an algorithm for this purpose.
Complex analysis via automated web tool
Their method combines the results of existing algorithms to obtain more precise and robust predictions of clinical subtypes. This unifies the characteristics and advantages of each algorithm and eliminates their time-consuming adjustment. “This makes it much easier to apply the analysis in clinical research,” reports Dr. Pauling. “For that reason, we have developed a web-based tool that permits online analysis of molecular clinical data by practitioners without prior knowledge of bioinformatics.”
On the website (https://exbio.wzw.tum.de/mosbi/), researchers can submit their data for automated analysis and use the results to interpret their studies. “Another important aspect for us was the visualization of the results. Previous approaches were not capable of generating intuitive visualizations of relationships between patient groups, clinical factors and molecular signatures. This will change with the web-based visualization produced by our MoSBi tool,” says Tim Rose, a scientist at the TUM School of Life Sciences. MoSBi stands for “Molecular Signatures using Biclustering”. “Biclustering” is the name of the technology used by the algorithm.
Application for clinically relevant questions
With the tool, researchers can now, for example, represent data from cancer studies and simulations for various scenarios. They have already demonstrated the potential of their method in a large-scale clinical study. In a cooperative study conducted with researchers from the Max Planck Institute in Dresden, the Technical University of Dresden and the Kiel University Clinic, they studied the change in lipid metabolism in the liver of patients with non-alcoholic fatty liver disease (NAFLD).
This widespread disease is associated with obesity and diabetes. It develops from the non-alcoholic fatty liver (NAFL), in which lipids are deposited in liver cells, to non-alcoholic steatohepatitis (NASH), in which the liver becomes further inflamed, to liver cirrhosis and the formation of tumors. Apart from dietary adjustments, no treatments have been found to date. Because the disease is characterized and diagnosed by the accumulation of various lipids in the liver, it is important to understand their molecular composition.
Biomarkers for liver disease
Using the MoSBi methods, the researchers were able to demonstrate the heterogeneity of the livers of patients in the NAFL stage at the molecular level. “From a molecular standpoint, the liver cells of many NAFL patients were almost identical to those of NASH patients, while others were still largely similar to healthy patients. We could also confirm our predictions using clinical data,” says Dr. Pauling. “We were then able to identify two potential lipid biomarkers for disease progression.” This is important for early recognition of the disease and its progression and the development of targeted treatments.
The research group is already working on further applications of their method to gain a better understanding of other diseases. “In the future algorithms will play an even greater role in biomedical research than they already do today. They can make it significantly easier to detect complex mechanisms and find more targeted treatment approaches,” says Dr. Pauling.