Anti-inflammatory drugs can help block hypertension-related kidney damage
anti-inflammatory drugs appear to help block the rapid kidney destruction that can occur with hypertension, Medical College of Georgia researchers report. Treating hypertensive rats with the broad-acting anti-inflammatory drug pentosan polysulfate preserves the kidney's ability to regulate pressure placed on tiny filters called glomeruli, they report in the American Journal of Physiology – Renal Physiology. A million of these fragile structures are responsible for filtering the body's total plasma volume 60 times daily.
Therapeutic intervention is a long-term goal, said Dr. Edward W. Inscho, corresponding author and physiologist in the MCG Schools of Graduate Studies and Medicine "Because the job is big, the kidneys are vulnerable to injury. If we can keep them functioning longer, quality of life is going to be better longer." But he notes that this exact approach isn't a treatment option primarily because of side effects that can result from long-term use of anti-inflammatory drugs.
Hypertension and diabetes take a similar toll on kidneys and together, the pervasive conditions are creating a rapidly growing number of patients in kidney failure. "The number of people going to dialysis because of these two maladies just grows exponentially so there is a really good reason to figure this out," said Inscho, who recently received a $1.8 million, five-year grant from the National Heart, Lung and Blood Institute to help do just that.
In a rather vicious circle, kidneys are hurt by and contribute to hypertension; which comes first remains unresolved. But one key way hypertension hurts kidneys is by blunting the function of afferent arterioles, tiny blood vessels that feed the filtering units.
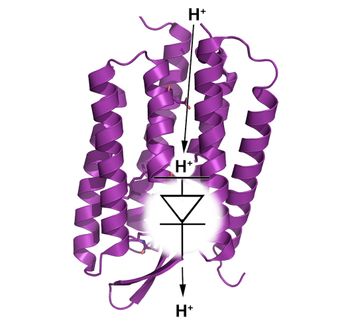
Much like a dam operator controls water flow into a river, a mechanosensor, likely located inside the smooth muscle cells that form the blood vessel walls, keeps tabs on the pressure of the blood flowing through the afferent arteriolar into the filters. If pressure gets too high, it prompts the small vessel to contract.
"You want the vasculature to constrict because filters are very delicate and the kidneys want to keep blood flow and filtration relatively constant," said Inscho noting that this balancing act enables kidney tubules, which reabsorb good things like glucose and amino acids, to do their job.
His animal studies have shown that mechanosensor function falters after just three days of high blood pressure. "The blood vessel does not seem to recognize the blood pressure increase," Inscho said. Even slightly elevated pressures resulting from too much salt consumption can render them less responsive but, at least initially, not lost. Rather the vessel's ability to sense and respond to pressure seems inactivated: when Inscho applies a vasoconstrictor agent directly onto the afferent arteriole, for example, it contracts. In the face of regular anti-inflammatory therapy, he's finding it retains the ability to sense pressure change and respond appropriately.
Inscho's new grant will help sort through just how the kidneys autoregulate pressure in normal scenarios, such as the typical blood pressure fluctuations that occur in healthy people throughout the day. He also wants to study the role the inflammatory factors TGF-beta and MCP-1 play in arteriole dysregulation. Both factors are elevated in high blood pressure and implicated in other types of vascular injury. Preliminary evidence suggests a strong link; that the factors set up some sort of signaling event that turns mechanosensors off or at least down. Ironically, impaired autoregulation leads to increased production of the inflammatory factors.
"We have data that argue that TGF-beta can definitely cause these blood vessels to fail," Inscho said. "If you apply the cytokine to a healthy kidney, the blood vessel will not respond correctly; wash it off and it does. Now we also have data that if we protect the kidneys from MCP-1, we can improve the function of these vessels."
He's looking at the impact of anti-inflammatory drugs pentosan polysulfate as well as mycophenolate mofetil because of existing evidence that their use reduces protein excretion in the urine, a sign of kidney damage. Rather than as a potential therapy, he views the drugs as tools for helping dissect a complex process.
"Hypertension-related kidney damage is multifaceted, but part of that cascade of progression to injury is functional impairment of that blood vessel. We have established that, I think, unequivocally," Inscho said. "The grant will enable us to get more information about normal function and pathology all at the same time."