A longer-lasting COVID vaccine?
Study points the way
Researchers at the Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research at UCLA have identified rare, naturally occurring T cells that are capable of targeting a protein found in SARS-CoV-2 and a range of other coronaviruses.
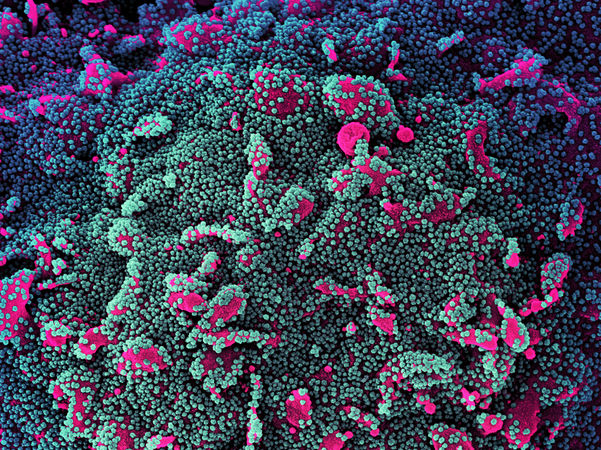
Microscope image showing a human cell (pink) heavily infected with SARS-CoV-2 virus particles (green and purple).
NIAID/NIH
The findings suggest that a component of this protein, called viral polymerase, could potentially be added to COVID-19 vaccines to create a longer-lasting immune response and increase protection against new variants of the virus.
Background
Most COVID-19 vaccines use part of the spike protein found on the surface of the virus to prompt the immune system to produce antibodies. However, newer variants — such as delta and omicron — carry mutations to the spike protein, which can make them less recognizable to the immune cells and antibodies stimulated by vaccination. Researchers say that a new generation of vaccines will likely be needed to create a more robust and wide-ranging immune response capable of beating back current variants and those that may arise in the future.
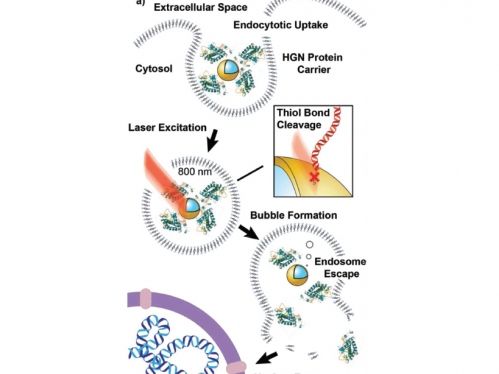
One way to accomplish this is by adding a fragment of a different viral protein to vaccines — one that is less prone to mutations than the spike protein and that will activate the immune system’s T cells. T cells are equipped with molecular receptors on their surfaces that recognize foreign protein fragments called antigens. When a T cell encounters an antigen its receptor recognizes, it self-replicates and produces additional immune cells, some of which target and kill infected cells immediately and others which remain in the body for decades to fight that same infection should it ever return.
Method
The researchers focused on the viral polymerase protein, which is found not only in SARS-CoV-2 but in other coronaviruses, including those that cause SARS, MERS and the common cold. Viral polymerases serve as engines that coronaviruses use to make copies of themselves, enabling infection to spread. Unlike the spike protein, viral polymerases are unlikely to change or mutate, even as viruses evolve.
To determine whether or not the human immune system has T cell receptors capable of recognizing viral polymerase, the researchers exposed blood samples from healthy human donors (collected prior to the COVID-19 pandemic) to the viral polymerase antigen. They found that certain T cell receptors did, in fact, recognize the polymerase. They then used a method they developed called CLInt-Seq to genetically sequence these receptors. Next, the researchers engineered T cells to carry these polymerase-targeting receptors, which enabled them to study the receptors’ ability to recognize and kill SARS-CoV-2 and other coronaviruses.
Impact
More than 5 million people have died from COVID-19 worldwide. Current vaccines provide significant protection against severe disease, but as new, potentially more contagious variants emerge, researchers recognize that vaccines may need to be updated — and the new UCLA findings point toward a strategy that may help increase protection and long-term immunity. The researchers are now conducting further studies to evaluate viral polymerase as a potential new vaccine component.
Original publication
Other news from the department science

Get the life science industry in your inbox
By submitting this form you agree that LUMITOS AG will send you the newsletter(s) selected above by email. Your data will not be passed on to third parties. Your data will be stored and processed in accordance with our data protection regulations. LUMITOS may contact you by email for the purpose of advertising or market and opinion surveys. You can revoke your consent at any time without giving reasons to LUMITOS AG, Ernst-Augustin-Str. 2, 12489 Berlin, Germany or by e-mail at revoke@lumitos.com with effect for the future. In addition, each email contains a link to unsubscribe from the corresponding newsletter.
Most read news
More news from our other portals
Last viewed contents
Transgene's Therapeutic Vaccine TG4010 Shows Promising Preliminary Phase IIbData in Advanced Non-Small Cell Lung Cancer
Better Genome Editing - Method giving complete spatiotemporal control and treads DNA lightly
Sensitive new assay detects hepatitis B infection in single liver cells and serum

Phidea S.r.l. - Corsico, Italy
Bavarian Nordic Announces Start of Randomized Phase 2 Study Comparing PROSTVAC and Chemotherapy versus Chemotherapy
NovAliX Enters into Multi-Target Integrated Drug Discovery Collaboration with Teijin Pharma
Santalum_album

Only alcohol -- not caffeine, diet or lack of sleep -- might trigger heart rhythm condition - Lifestyle factors may play role in managing the malady, latest study shows
Medgenics appoints Lord Steinberg as Non-Exec Director