Protein from the liver may cause Alzheimer’s disease in the brain
Peripherally produced amyloid causes neurodegeneration
Amyloid protein made in the liver can cause neurodegeneration in the brain, according to a new study in the open-access journal PLOS Biology, by John Mamo of Curtin University in Bentley, Australia, and colleagues. Since the protein is thought to be a key contributor to development of Alzheimer’s disease (AD), the results suggest that the liver may play an important role in the onset or progression of the disease.
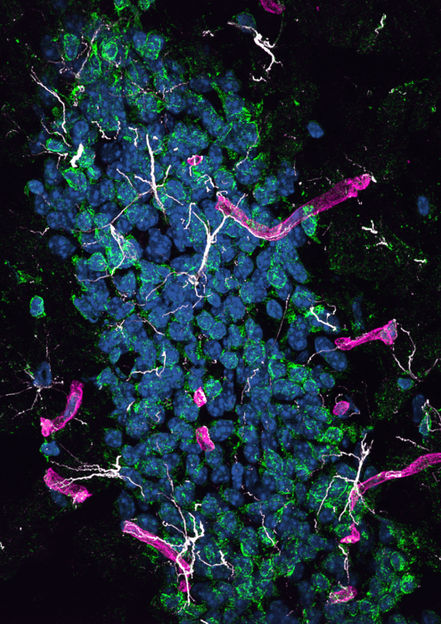
Hippocampal dentate gyrus in HSHA mice, showing significant astrocyte activation (GFAP: white) and oxidative stress (8OHdG: green) surrounding the cerebral capillaries (laminin-a4: magenta). Nuclei staining with DAPI (blue).
John Charles Louis Mamo, Lam V et al., 2021, PLOS Biology, CC BY 4.0 (https://creativecommons.org/licenses/by/4.0/)
Deposits of amyloid-beta (A-beta) in the brain are one of the pathological hallmarks of AD and are implicated in neurodegeneration in both human patients and animal models of the disease. But A-beta is also present in periphereral organs, and blood levels of A-beta correlate with cerebral amyloid burden and cognitive decline, raising the possibility that peripherally produced a-beta may contribute to the disease. Testing that hypothesis has been difficult, since the brain also produces A-beta, and distinguishing protein from the two sources is challenging.
In the current study, the authors surmounted that challenge by developing a mouse that produces human a-beta only in liver cells. They showed that the protein was carried in the blood by triglyceride-rich lipoproteins, just as it is in humans, and passed from the periphery into the brain. They found that mice developed neurodegeneration and brain atrophy, which was accompanied by neurovascular inflammation and dysfunction of cerebral capillaries, both commonly observed with Alzheimer’s disease. Affected mice performed poorly on a learning test that depends on function of the hippocampus, the brain structure that is essential for the formation of new memories.
The findings from this study indicate that peripherally derived A-beta has the ability to cause neurodegeneration and suggest that A-beta made in the liver is a potential contributor to human disease. If that contribution is significant, the findings may have major implications for understanding Alzheimer’s disease. To date, most models of the disease have focused on brain overproduction of A-beta, which mimics the rare genetic cases of human Alzheimer’s. But for the vast majority of AD cases, overproduction of A-beta in the brain is not thought to be central to the disease etiology. Instead, lifestyle factors may play a more important role, including a high-fat diet, which might accelerate liver production of A-beta.
The effects of peripheral A-beta on brain capillaries may be critical in the disease process, Mamo adds. “While further studies are now needed, this finding shows the abundance of these toxic protein deposits in the blood could potentially be addressed through a person’s diet and some drugs that could specifically target lipoprotein amyloid, therefore reducing their risk or slowing the progression of Alzheimer’s disease.”
Original publication
Most read news
Original publication
Lam V, Takechi R, Hackett MJ, Francis R, Bynevelt M, Celliers LM, et al.; "Synthesis of human amyloid restricted to liver results in an Alzheimer disease–like neurodegenerative phenotype"; PLoS Biol; 2021, 19(9): e3001358.
Organizations
Other news from the department science

Get the life science industry in your inbox
By submitting this form you agree that LUMITOS AG will send you the newsletter(s) selected above by email. Your data will not be passed on to third parties. Your data will be stored and processed in accordance with our data protection regulations. LUMITOS may contact you by email for the purpose of advertising or market and opinion surveys. You can revoke your consent at any time without giving reasons to LUMITOS AG, Ernst-Augustin-Str. 2, 12489 Berlin, Germany or by e-mail at revoke@lumitos.com with effect for the future. In addition, each email contains a link to unsubscribe from the corresponding newsletter.