Does immunothrombosis make the coronavirus especially dangerous?
Researchers investigate disease progression in severe SARS-CoV2 cases
Advertisement
By mid-2020, the coronavirus caused more than 600,000 deaths worldwide. The processes in the body that make a SARS-CoV2 infection so dangerous have not yet been fully clarified. A research team led by Dr. med. Moritz Leppkes of FAU has now discovered that in Covid-19 infections certain white blood cells, the neutrophilic granulocytes, are activated particularly aggressively, and then agglomerate and form nets known as neutrophil extracellular traps (NETs) in the blood vessels of the lungs. The blood vessels become clogged not only through coagulation, but also by immunological processes, which the researchers call immunothrombosis. As a consequence of the immunological processes, the oxygen supply and the gas exchange in the body are no longer ensured, which leads to severe progression of the disease.
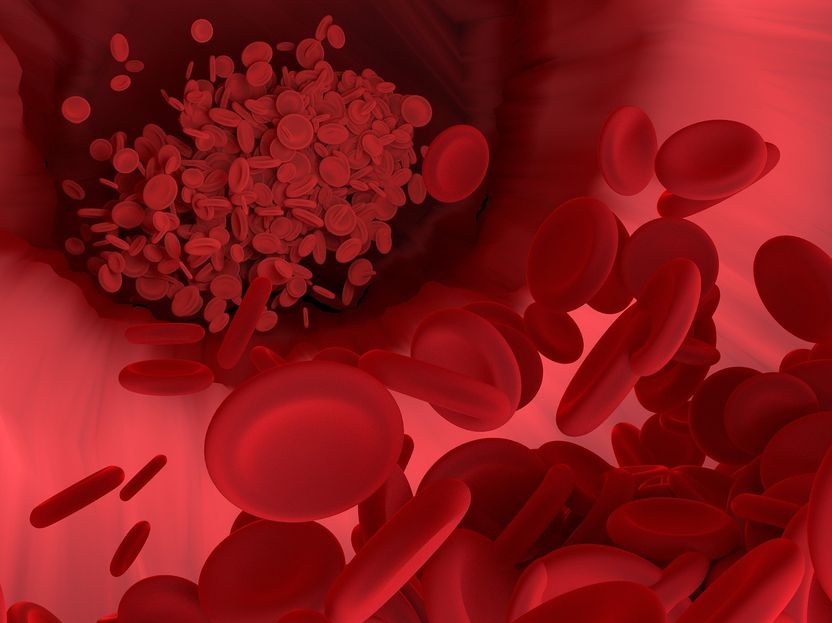
Symbolic image
Vector8DIY, pixabay.com
Fast closure of the smallest pulmonary vessels
The increased agglomeration of neutrophilic granulocytes and the subsequent NET formation are presumably caused in Covid-19 by viral damage to the endothelium, the lining of the blood vessels. The endothelial cells, like the cells of the pulmonary vesicles, are rich in ACE2, a receptor for the coronavirus. The virus docks onto the cells and damages them. Endothelial damage in turn attracts neutrophilc granulocytes, which play an important role in immune defence. In the case of a SARS-CoV2 infection, as the team led by Dr. Leppkes discovered, a special form of these immune cells is increasingly being formed – neutrophilic granulocytes of low density, which are increasingly prone to NET formation and also play a role in autoimmune processes. In an autoimmune response, the immune system is directed against the body.
In addition to blood coagulation and thromboses caused by platelets, all these mechanisms lead to blockage, in particular of the small and smallest blood vessels of the lungs. Although to some extent NET formation in inflammation is a normal part of pathogen defence, in Covid-19 this process is not limited to one area of an organ, but occurs in many blood vessels, including various organs. This is particularly threatening because the microvessels of the lungs close quickly.
Among other things, the researchers gained their insights through the immunohistochemical analysis of autopsy material and blood samples from Covid-19 patients, which they compared with samples from healthy and less severely ill patients.
Possible approaches to treatment
Researchers see a treatment approach in severe Covid-19 cases as inhibiting the agglomeration of neutrophilic granulocytes and preventing increased NET formation. This could be done, for example, by dexamethasone, which inhibits cell aggregation, and by active substances which counteract NET formation, for example by attacking PAD4 enzymes. FAU researchers also observed a hitherto neglected function of the blood coagulation inhibitor heparin, which supports the breakdown of NETs and thus improves blood circulation.