Too much of a good thing: overactive immune cells trigger inflammation
Scientists describe a previously unknown disorder of the immune system: in a distinct subset of immune cells from patients with primary immunodeficiency, cellular respiration is significantly increased. This cellular metabolic overactivity leads to inflammation, as an international research team led by the University of Basel and University Hospital Basel report in the journal Nature Immunology.
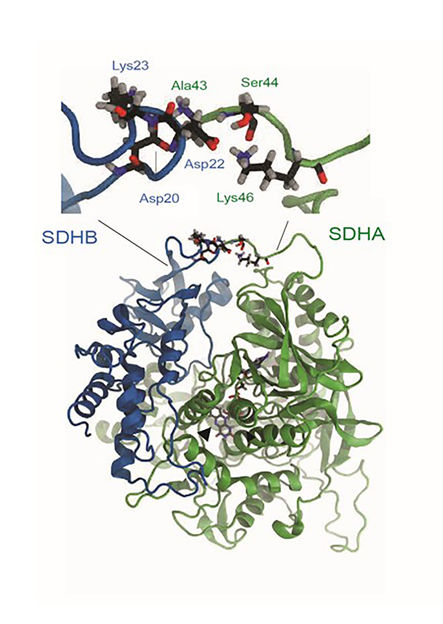
Molecular model: A typical interaction between the A45T mutated SDHA gene (green) and the SDHB gene (blue).
DBM
The immune system protects us from infections and tumors – a challenging task, not least because harming the body’s own healthy tissue must be avoided at the same time. However, rare genetic diseases lead to defects in the immune system known as primary immunodeficiency disorders (PID). One consequence of such disorders is susceptibility to infections, yet certain tumors and non-infectious inflammation (autoimmune diseases) can also occur more frequently.
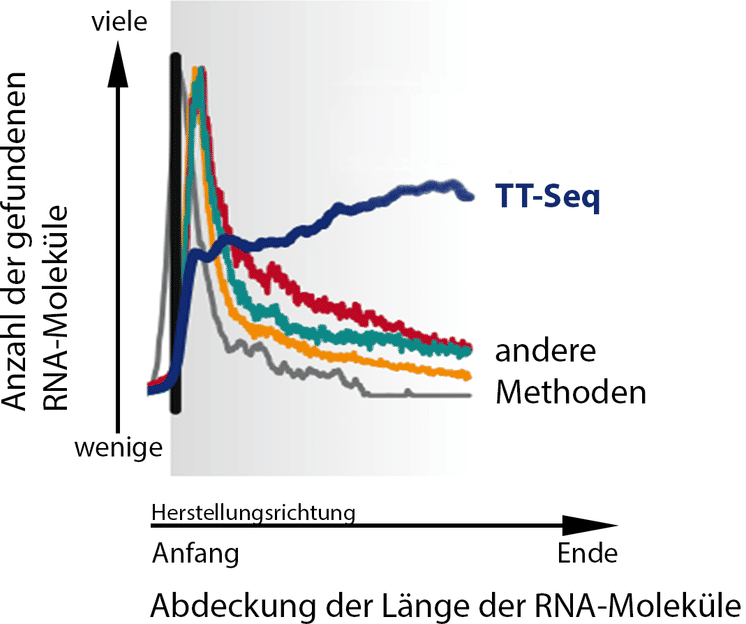
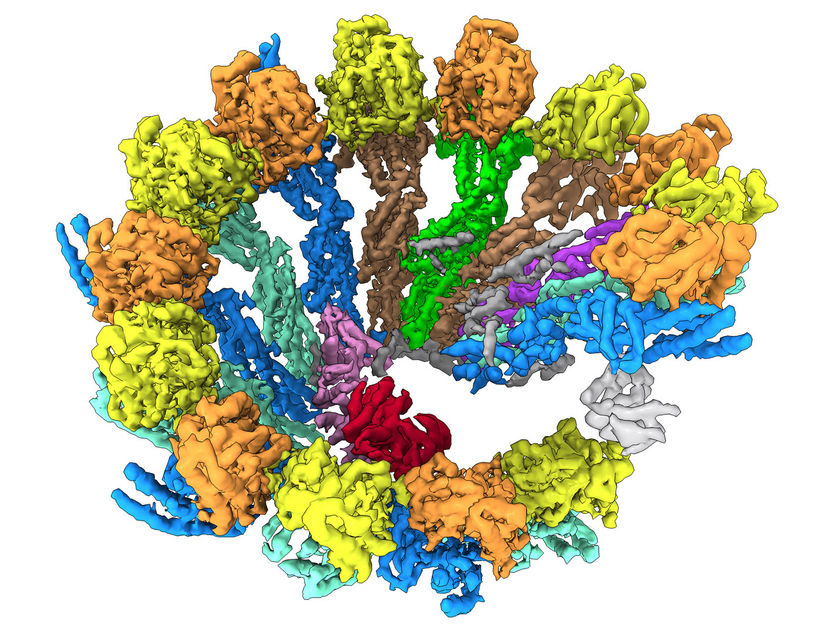
The researchers tested the hypothesis that the metabolic activity in the immune cells of PID patients can serve as a biomarker. They based this on the fact that cellular metabolism is a key regulator of the functioning of immune cells. In the immune cells of a subset of the examined PID patients, a key metabolic process – cellular respiration – was indeed significantly increased. During cellular respiration, energy is generated in the mitochondria, the “powerhouses of the cell”.
Increased cellular respiration
On the basis of this discovery, the researchers were able to decode a new kind of disease mechanism, from the genetic defect via mitochondria and back to signal transduction to the nucleus. The increased cellular respiration was triggered by the hyperactivity of a protein in the respiratory chain. This then signaled the cells to produce inflammatory mediators. With these findings, the researchers were able to successfully administer a targeted treatment approved for another indication.
The study was led by Professor Christoph Hess (Department of Biomedicine (DBM) of the University of Basel and University Hospital Basel, and CITIID, University of Cambridge) and Professor Mike Recher (DBM, University of Basel and University Hospital Basel). “It is an example of how patient-based research can help to decode disease-causing molecular processes,” Christoph Hess says. This benefits patients, who may receive more targeted and effective medication with fewer side effects. Further, insights into fundamental biological processes gained from studying rare diseases can also enable new pathophysiological considerations relating to more common diseases.
Original publication
Other news from the department science

Get the life science industry in your inbox
By submitting this form you agree that LUMITOS AG will send you the newsletter(s) selected above by email. Your data will not be passed on to third parties. Your data will be stored and processed in accordance with our data protection regulations. LUMITOS may contact you by email for the purpose of advertising or market and opinion surveys. You can revoke your consent at any time without giving reasons to LUMITOS AG, Ernst-Augustin-Str. 2, 12489 Berlin, Germany or by e-mail at revoke@lumitos.com with effect for the future. In addition, each email contains a link to unsubscribe from the corresponding newsletter.
Most read news
More news from our other portals
Last viewed contents
Tea
N-Phenethyl-4-piperidinone
How Cells Assemble Their Skeleton - Researchers study the formation of microtubules
Biopower
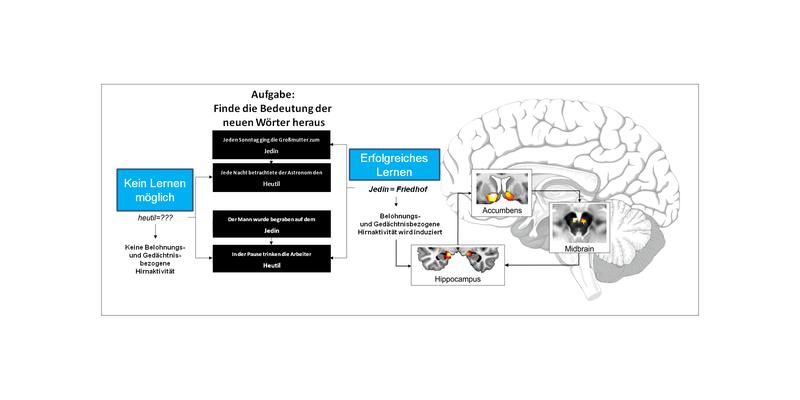
When learning is fun - How the brain simulates external rewards to boost memory formation
Category:Brain_Tumor_Funders'_Collaborative
Category:Hormones_of_the_hypothalamo-pituitary_system
ZAKA
American_Lebanese_Syrian_Associated_Charities
Panaeolus_tropicalis