Scars: gone with the foam
Prevent excessive scarring
Poorly healing wounds and severe scarring are more than just a cosmetic problem; they can significantly impair a person's mobility and health. Empa researchers have now developed a foam that is supposed to prevent excessive scarring and help wounds to heal quickly. An essential ingredient: the yellow ginger tumeric.
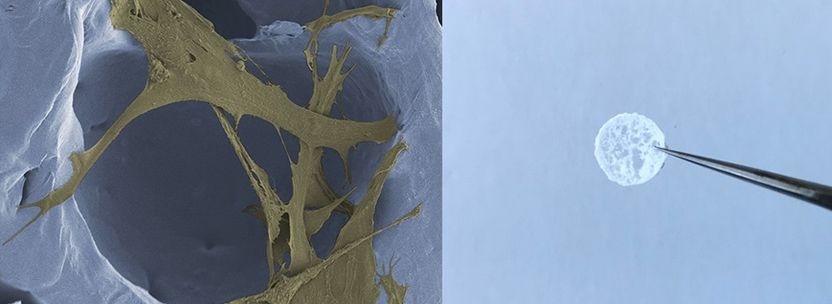
The foam can be placed in skin wounds and supports the natural healing process (right). In the scaffold of the polymer foam cells like these fibroblasts find a good hold to build up new skin tissue (left).
Empa
A scar on the elbow that is strained with every movement, or a foot, on which a wound simply does not want to close – poorly healing injuries are a common cause of health restrictions. And although millions of people are affected in their everyday lives, the complex process of wound healing is not yet fully understood, let alone controllable. Empa researchers have, therefore, developed a foam that is supposed to be placed in skin wounds to support and optimize the natural healing process. With the "Scaravoid" project, Markus Rottmar and his team in Empa's Biointerfaces lab have taken a step in a new direction. "Traditional treatments target individual factors of wound healing, such as oxygen supply or moisture regulation, and only produce an inadequate tissue response," explains Rottmar. Within "Scaravoid", which is sponsored by the Gebert Rüf Foundation, the healing process is to be understood and supported more comprehensively.
Perfectly orchestrated
It is clear so far that a perfectly orchestrated interaction of numerous individual factors in the body is necessary in order to close a skin injury and transform it into healthy tissue. Cells must be attracted so that a well-dosed inflammation cleanses the wound. In order for the cleaned defect to close, new tissue grows, which is then transformed into functional skin. As astonishing as the body's self-healing powers are, a malfunction can disturb the balance and lead to excessive scarring or inadequate wound closure. In older people or diabetics, for instance, the risk that the complex cascade may be impaired is increased.
With "Scaravoid", the Empa team is now intervening at several stages in the process thanks to a biological polymer scaffold that is already approved for certain medical uses. In a high-pressure reactor, the polymer is expanded using supercritical carbon dioxide (CO2), whereby the pore size can be finely tuned by varying pressure and temperature. Once placed in a wound, the polymer scaffold is to begin its work: With its open-pored architecture, it offers immigrant cells a suitable structure to settle in. Since the foam is biodegradable, the cells disintegrate the polymer structure and produce a new scaffold according to their needs to form a new, functional tissue.
Natural balance
In order to prevent undesired scarring, the polymer scaffold is equipped with a bioactive substance that is supposed to inhibit scarring. The researchers use a substance that is known way better from the kitchen than from the hospital: curcumin. The powder of the turmeric root, also known as yellow ginger, is an E100 additive that dyes foods such as mustard or margarine and contributes to the taste of curry powder. Curcumin, on the other hand, is an interesting pharmacological component because of its anti-inflammatory characteristics. The Empa researchers added curcumin to cell cultures and found that the production of biomarkers typically found in scars is significantly reduced.
In the foam, curcumin is bound inside the scaffold and is gradually released. It controls the behavior and function of the cells that migrate into the scaffold and thus supports the natural balance of wound healing. What is currently being analyzed in lab tests in the form of small polymer discs will be used in clinical trials in the form of larger polymer membranes. The membranes can be cut to size by the physician and placed into the wound. The membranes are intended to optimize wound healing, particularly in the event of serious injuries, such as those following traffic accidents or severe burns.
Most read news
Organizations
Other news from the department science

Get the life science industry in your inbox
By submitting this form you agree that LUMITOS AG will send you the newsletter(s) selected above by email. Your data will not be passed on to third parties. Your data will be stored and processed in accordance with our data protection regulations. LUMITOS may contact you by email for the purpose of advertising or market and opinion surveys. You can revoke your consent at any time without giving reasons to LUMITOS AG, Ernst-Augustin-Str. 2, 12489 Berlin, Germany or by e-mail at revoke@lumitos.com with effect for the future. In addition, each email contains a link to unsubscribe from the corresponding newsletter.


















































