Successful T cell engineering with gene scissors
CRISPR/Cas9-modified T cells could solve immunotherapy problems
The idea of genetically modifying a patient’s own immune cells and deploying them against infections and tumors has been around since the 1980s. But to this day modified T cells are still not as effective as natural T cells and have been only been of limited clinical value. Using the new CRISPR-Cas9 gene editing tool, a team at the Technical University of Munich (TUM) has now engineered T cells that are very similar to physiological immune cells.

The study team of the Institute for Medical Microbiology, Immunology and Hygiene (from left to right): Prof. Dirk Busch, Thomas Müller and Kilian Schober
K. Schober / TUM
There are two forms of T cell therapy: either a recipient receives cells from a donor, or the recipient’s own T cells are removed, genetically reprogrammed in a laboratory and unleashed against an infection or tumor in the body. While the first method has proven to be successful in clinical models, reprogramming T cells is still beset with problems.
Modifying T cell receptors
The team led by Professor Dirk Busch, Director of the Institute for Medical Microbiology, Immunology and Hygiene at the TUM, has generated modified T cells for the first time that are very similar to their natural counterparts and could solve some of those problems. To do so, they utilized the new CRISPR-Cas9 gene scissors, which can be used to snip out and replace targeted segments of the genome.
Both the conventional methods and the new method target the key homing instrument of T cells, known as the T cell receptor. The receptor, residing on the cell’s surface, recognizes specific antigens associated with pathogens or tumor cells, which the T cell is then able to attack. Each receptor is made up of two molecular chains that are linked together. The genetic information for the chains can be genetically modified to produce new receptors that are able to recognize any desired antigen. In this way, it is possible to reprogram T cells.
Targeted exchange using the CRISPR-Cas9 gene scissors
The problem with conventional methods is that the genetic information for the new receptors is randomly inserted into the genome. This means that T cells are produced with both new and old receptors or with receptors having one old and one new chain. As a result, the cells do not function as effectively as physiological T cells and are also controlled differently. Moreover, there is a danger that the mixed chains could trigger dangerous side effects (Graft-versus-Host Disease, GvHD).
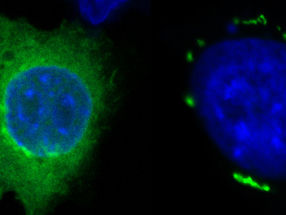
“Using the CRISPR method, we’ve been able to completely replace the natural receptors with new ones, because we’re able to insert them into the very same location in the genome. In addition, we’ve replaced the information for both chains so that there are no longer any mixed receptors,” explains Kilian Schober, who is a lead author of the new study along with his colleague Thomas Müller.
Near-natural properties
Thomas Müller explains the advantages of the modified T cells: “They’re much more similar to physiological T cells, yet they can be changed flexibly. They’re controlled like physiological cells and have the same structure, but are capable of being genetically modified.“ The scientists have demonstrated in a cell culture model that T cells modified in this way behave nearly exactly like their natural counterparts.
“Another advantage is that the new method allows multiple T cells to be modified simultaneously so that they’re able to recognize different targets and can be used in combination. This is especially interesting for cancer therapy, because tumors are highly heterogeneous,” Dirk Busch adds. In the future, the team plans to investigate the new cells and their properties in preclinical mouse models, an important step in preparing for clinical trials with humans.
Original publication
Kilian Schober, Thomas R. Müller, Füsun Gökmen, Simon Grassmann, Manuel Effenberger, Mateusz Poltorak, Christian Stemberger, Kathrin Schumann, Theodore L. Roth, Alexander Marson and Dirk H. Busch; "Orthotopic replacement of T-cell receptor ɑ- and β-chains with preservation of near-physiological"; Nature Biomedical Engineering; June 12, 2019