Cell recycling to fight atherosclerosis
Advertisement
Calcium deposits in the abdominal and leg arteries – so-called media calcification – are a frequent complication of kidney failure or diabetes mellitus. With the support of the Austrian Science Fund FWF, researchers explored how cell cultures and mice react to inadequate blood purification and how to prevent the ossification of vascular walls.
In time with the beating of our heart, our arteries transport oxygen-rich blood through the body. If these arterial muscle tubes change in structure or become clogged, serious complications will ensue. Atherosclerosis is one such well-known phenomenon that results in heart attacks or strokes. In people with chronic kidney failure, but also in long-term diabetics, vascular calcification is a frequent complication. In this case, it is not primarily the inner wall of the artery that is affected, but the middle layer of the vessel, hence the name media calcification. One underlying cause is the high phosphate or sugar content in the patients’ blood, and the micro-milieu in the tissue itself also plays a role. “In the preliminary work for our project, we were able to show that the abdominal aorta tends to calcify more than the thoracic aorta,” explains Philipp Eller from the Department of Internal Medicine at the Medical University of Graz. Supported by the Austrian Science Fund FWF, a team from the Medical University headed by Eller searched for drivers and protective mechanisms as well as therapeutic possibilities of counteracting vascular ossification.
Fantastic vascular plasticity
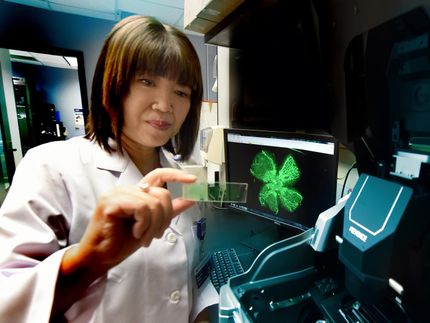
Arteries consist of smooth muscle cells that are not fully differentiated, which enables them to react plastically to injuries or stress, i.e. to adapt functionally. The range of arterial reactions depends largely on their history, because the thoracic and abdominal arteries, for example, develop from different germ layers during embryonic development. The smooth muscle cells of the abdominal artery therefore have the ability to behave like bone cells. In the search for protective factors and drivers of media calcification, Philipp Eller and his team worked with mice as model organisms and with muscle cell cultures they examined for histopathological and molecular aspects. In the mice, kidney failure (uraemia) was induced with a high-phosphate diet. A calcification environment was also simulated for the cell culture, and the ossification was quantified by mass spectrometry.
Two protective approaches at once
A comparison of gene activity in mice fed a normal diet and mice fed a phosphate-rich diet revealed two striking patterns. Genes responsible for a cellular disposal and recycling mechanism, a phenomenon known as autophagy, were particularly active. The team also observed that media calcification was associated with an altered microRNA production. The most surprising result for principal investigator Eller was that autophagy acts as a protective mechanism against vascular calcification, which could be shown both in vitro and in vivo. Autophagy is a process mastered by all cells: defective and unnecessary cell components are encapsulated and broken down into reusable building blocks. In this specific case, drug-induced autophagy counteracts calcification.
In preclinical tests, the mice that had been given autophagy-inducing drugs survived longer. In a parallel test, the team explored whether the administration of microRNA-142-3p improves the elasticity of the vessels, i.e. whether it counteracts the stiffening of vessels by calcification. In order to manage the interdisciplinary range of test settings and ensure the solid checking of results, various departments of the Medical University of Graz collaborated with a partner university in Maribor. Both experimental approaches point towards possible pharmacological therapy concepts against media calcification, which are now being subjected to further investigations. In a follow-up project, an attempt will be made to stimulate the autophagy mechanism with drugs that have fewer side effects.
Original publication
Máté Kétszeri, Andrijana Kirsch, Bianca Frauscher et al.; "MicroRNA-142-3p improves vascular relaxation in uremia"; Atherosclerosis 280, 2019