Fight-or-flight hormones help tumor cells escape to spread
Chronic stress triggers a chain of molecular events that protects breakaway ovarian cancer cells from destruction, a team of researchers led by scientists at The University of Texas M. D. Anderson Cancer Center reports in the Journal of Clinical Investigation.
In preclinical research, the team found that heightened levels of the fight-or-flight stress hormones epinephrine and norepinephrine permit more malignant cells to safely leave the primary tumor, a necessary step in metastasis and cancer progression. They also found that ovarian cancer patients face earlier mortality when a crucial protein activated by the hormones is present at high levels in their tumors and that depressed patients have higher levels of the protein.
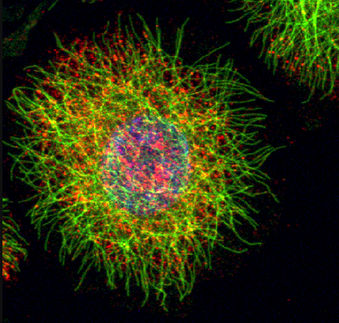
"When normal cells become detached from neighboring cells or from the supportive scaffolding known as the extracellular matrix, they die from anoikis, a form of programmed cell death," said first author Anil Sood, M.D., professor in M. D. Anderson's Departments of Gynecologic Oncology and Cancer Biology.
"Cancer cells find a way to bypass anoikis, so they survive as individual cells circulating in the blood or in ascites, fluid that accumulates in the abdomen of ovarian cancer patients," Sood said. Resistance to cell death helps malignant cells migrate from the primary tumor and re-attach to colonize new sites.
"Restoring cancer cells' vulnerability to anoikis would open a new avenue for suppressing tumor growth and metastasis," Sood said. Two promising approaches - directly silencing a crucial protein or using beta blockers to preempt its activation - worked in cell culture and mouse models, making them candidates for human use.
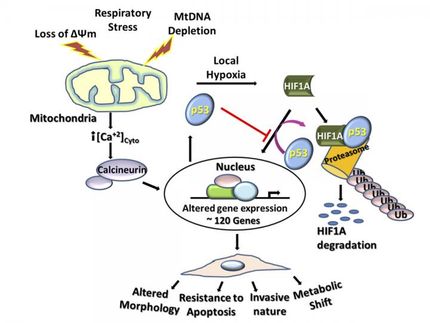
The team showed that increases in epinephrine, also known as adrenaline, and norepinephrine reduced the number of ovarian cancer cells killed by anoikis by activating focal adhesion kinase (FAK), a protein known to promote tumor survival and to protect against anoikis. The researchers previously showed that FAK is abundantly present in ovarian cancer cells.
Lab experiments showed that resistance to cell death by anoikis begins when one of the hormones connects with the ß2-adrenergic receptor (ADRB2), which activates FAK via other intermediate proteins. Treating cells with beta blockers to inhibit the ADRB2 connection or using small interfering RNA (siRNA) to shut down FAK increased cell death.
In a mouse model of human ovarian cancer, mice subject to restraint stress had smaller tumors with fewer nodules and greater cell death when treated with siRNA to suppress FAK. Treatment with the beta blocker propranolol had a similar effect.
The researchers examined 80 cases of invasive epithelial ovarian cancer to assess the role of stress-induced FAK activity. They found increased FAK expression in 67 percent of patients and heightened levels of phosphorylated FAK in 50 percent.
Patients with high levels of either measure had greatly reduced overall survival over three years. About 65 percent of those with low FAK expression survived at least three years compared with 30 percent of those with high expression. For activated FAK, the difference was 65 percent vs. about 15 percent.
Using depression as an indicator of stress, the researchers found major depression was associated with higher levels of activated FAK and increased levels of norepinephrine in the tumors. Major depression was defined as a score greater than 16 on the Center for Epidemiological Studies Depression [CESD] scale for the purposes of this study.
Sood said future research will include investigating whether similar effects occur in other types of cancer, prospectively assessing the significance of FAK activation in chronic stress settings, and ultimately bringing strategies to clinical settings that can block the deleterious effects of chronic stress on tumor growth and progression.