Early in vitro testing for adverse effects on embryos
ETH researchers have combined embryonic cells and liver cells in a new cell culture test. This combination lets them detect adverse effects that new medications may have on embryos early on in the drug development process.
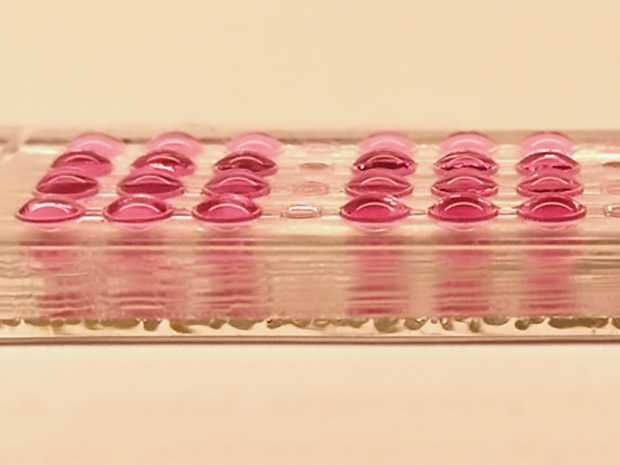
A chip with four rows of the new embryotoxicity test.
ETH Zürich / Julia Boos
Medications have to be safe for mothers-to-be and for their unborn children. Before the authorities will approve a new drug, it must be tested in animal trials on pregnant rodents and, as a rule, pregnant rabbits. Scientists in the Department of Biosystems Science and Engineering at ETH Zurich in Basel have now developed a test that allows them to examine a drug’s embryotoxicity in cell cultures instead of animals.
The new test does not yet replace the animal trials that are legally required as part of the medication approval process. However, as the new procedure is simple, fast, and inexpensive, researchers will be able to use it in the future to test a large number of drug candidates at an early stage of the development process. Substances that are harmful to embryos will thus be detected early in the drug development process and not only in embryotoxicity studies in animal trials. Because they are so expensive, animal tests are not conducted until much later in the drug development process with only carefully preselected potential drug candidates. As the new test weeds out unsuccessful drug candidates earlier, it may help cutting costs and reducing the number of animal experiments.
Cell culture test with stem cells
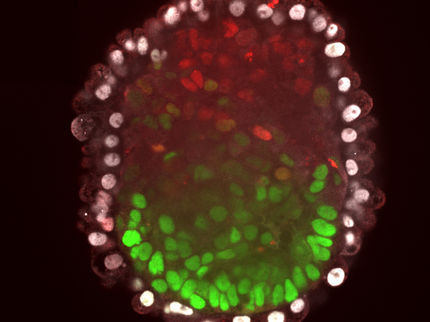
The new procedure is an advanced form of the embryonic stem cell test, in which substances are tested in vitro on so-called embryoid bodies. These three-dimensional clumps of cells are formed from embryonic stem cells – in this case, from a mouse – and undergo the first stages of embryonic development over a period of ten days. No viable embryos can be produced from these cells.
Led by ETH Professor Andreas Hierlemann, the research group has now expanded this embryonic stem cell test to include human liver tissue. “There’s a whole host of substances that are not toxic in their original form, but can be transformed into adverse substances by the human metabolism – especially by the liver,” explains Julia Boos, a doctoral student in Hierlemann’s group and lead author of the study, which has been published in the journal Advanced Science. In contrast to the conventional embryonic stem cell test, the newly developed test can detect substances of this nature.
Body on a chip
From beginning to end, the new test takes place in its entirety on a single cell-culture chip, which is equipped with various compartments. The compartments contain microtissue spheres, formed from human liver cells by the ETH spin-off InSphero, and embryoid bodies, grown from mouse stem cells. The liver microtissues and embryoid bodies have a diameter of about half a millimetre and are placed in different compartments, which are connected through microchannels to guarantee a constant liquid exchange between the different groups of cells.
“We’re the first to directly combine liver and embryonic cells in a body-on-a-chip approach,” Boos says. Just as a pregnant woman’s circulatory system links the metabolic processes in her liver with those in her developing embryo, this connected system ensures constant interaction between the liver cells and embryonic cells. “Metabolites created by the liver cells – including metabolites that are stable for just a few minutes – can thus act directly on the embryonic cells,” Boos says. She explains that combining the two in a single chip presents an improvement over other existing in vitro tests, which investigate the metabolisation of substances in the liver separately from the effects that these metabolites have on embryonic cells.
Boos goes on to describe another advantage of the new test: “In contrast to tests on living pregnant mice, in our test, the substances are metabolised by human liver cells – in other words, just as they would be in the human body when the medication is administered.” She points out that this is relevant, as humans and mice have different metabolisms.
Further development for high-throughput testing
The researchers demonstrated the effectiveness of the new test with the help of cyclophosphamide. This chemotherapeutic drug has virtually no effect in its basic form, but the liver transforms it into a substance that is toxic to cells. Two tests were run with cyclophosphamide: one included the newly developed liver/embryoid body test, and the other involved embryoid bodies alone without liver microtissues. What these tests revealed was that a fourfold lower concentration of cyclophosphamide was enough to have an adverse effect on the development of the embryoid bodies when liver tissue was present in the same environment.
Now, the scientists need to refine the test further before it can be applied in drug development. They are paying particular attention to the materials that are used in the test in addition to how well the procedures can be automated. Automation would be necessary if the pharmaceutical industry or other researchers were to be able to deploy the test on a large scale for high-throughput screening of drug candidates. In addition, the scientists wish to develop a test that uses reprogrammed human stem cells (known as iPS cells) instead of mouse stem cells. Then they would have an in vitro test entirely based on human tissue.