How can bacteria adapt to resist treatment by antibiotics?
Advertisement
In a joint collaboration, researchers from Denmark and Switzerland have shown that bacteria produce a specific stress molecule, divide more slowly, and thus save energy when they are exposed to antibiotics. The new knowledge is expected to form the basis for development of a new type of antibiotics.
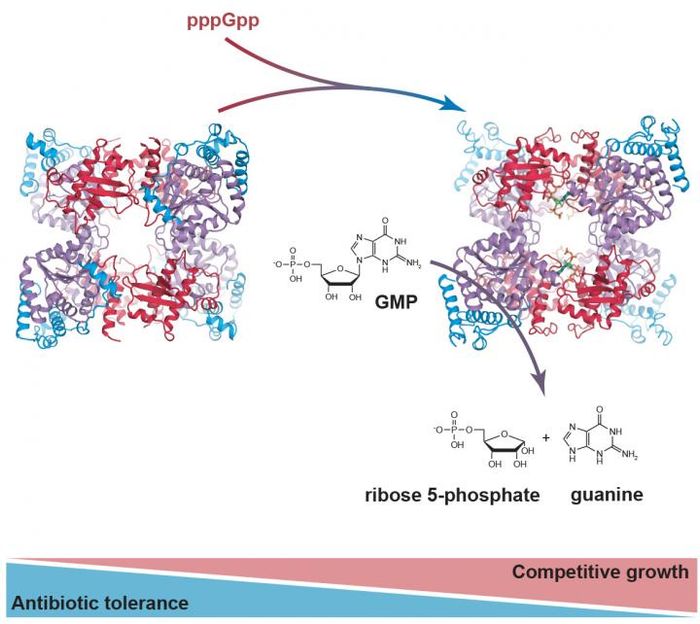
The figure shows how the enzyme PpnN binds pppGpp and speeds up conversion of guanylate (GMP) to its constituents ribose-5-phosphate and guanine. This enables bacteria to balance their tolerance towards antibiotics with the fitness requirements for survival (below).
Ditlev E. Brodersen/AU
All free-living organisms are under constant pressure to survive. Darwin dubbed this "survival of the fittest" and thus described how the best adapted species would have most offspring and therefore eventually end up propagating itself.
This fundamental principle is particularly prominent in the world of microorganisms, where free-living bacteria live in a constant fight to be the most well adapted and thus those who divide fastest in any given natural habitat. But when bacteria at the same time are exposed to deadly antibiotics, this fight becomes a question of balancing fitness, i.e. the ability to divide fast, with tolerance towards antibiotics. This amazing adaptability of bacteria is a contributing factor to the severity of infectious diseases in humans, including tuberculosis and severe urinary tract infection, for which the disease often resurfaces after treatment has ended.
In a new research paper, published in Molecular Cell, researchers from Aarhus University have collaborated with experts from the University of Copenhagen and the technical university ETH Zürich in Switzerland and taken a close look at how bacteria handle this difficult balancing act. The results show that bacteria very quickly reduce their rate of cell division when exposed to antibiotics in order to maintain the highest possible tolerance, but quickly start growing again when the substances are removed and fitness is the most important factor.
Bacteria save up energy
At the molecular level, the researchers in the group of Asc. Prof. Ditlev Egeskov Brodersen from the Department of Molecular Biology and Genetics at Aarhus University have been able to show that the effect is mediated by an enzyme within the bacteria, capable of saving up molecular energy in the form of constituents of cellular DNA, which can be used for rapid regrowth when the antibiotic treatment is ceased. When the bacteria are exposed to antibiotics, they immediately start breaking down substituents of DNA (the so-called nucleotides), into smaller parts that are then stored in the cell.
The researchers have shown that bacteria produce a specific stress molecule called (p)ppGpp upon exposure to antibiotics that makes the enzyme more active. This thus means that the saving up of energy happens extra fast when the bacteria are exposed to stress. Using an advanced analytical method called x-ray crystallography, the researchers have been able to generate detailed 3D pictures of the enzyme, both in its normal state and when bound to the stress molecule. The results surprisingly show that the enzyme opens up when the stress hormone is present, and thus functions much more efficiently because the nucleotides can more easily access the active site where the breakdown process takes place.
It is expected that the new knowledge about the molecular basis for the reaction of bacteria to antibiotics can be used to develop a whole new type of antibiotics that prevent bacteria from saving up energy and thus adapt to the treatment.