'Undruggable' Parkinson's molecule spills its secrets
Successful pharmacological activation of Nurr1 opens doors to novel therapies for incurable movement disorder
UC San Francisco researchers have for the first time developed a strategy for targeting a key molecule implicated in Parkinson's disease, opening up a potential new treatment strategy for the currently incurable movement disorder.
"This molecule is widely regarded as one of the top therapeutic targets for Parkinson's disease, but this is the first convincing evidence that it can be directly drugged," said Pamela England, PhD, an associate professor of pharmaceutical chemistry in UCSF's School of Pharmacy, and of cellular and molecular pharmacology in UCSF's School of Medicine, who was the senior author of the new study, published in Cell Chemical Biology .
Parkinson's disease affects 10 million people worldwide with progressively worsening movement difficulties as well as cognitive and mood-related symptoms, all of which are caused by degeneration of midbrain neurons that produce the neurotransmitter dopamine. For the vast majority of Parkinson's patients, their disease has no obvious genetic or environmental cause, and there is currently no treatment to prevent or slow the disease. Existing drugs only temporarily boost dopamine signaling to soften the disease's symptoms, and can lead to serious side effects.
Over the past decade, research has shown that before dopamine neurons begin to degenerate, they first stop making dopamine, suggesting that defects in the molecular pathway that produces and stores dopamine may be a culprit in the cells' eventual demise. A prime suspect in this chain of events is the transcription factor Nurr1, a gene-activating protein that is critical for the survival of dopamine neurons, and also regulates many aspects of their dopamine production and storage. Research in genetically modified mice has found that too little Nurr1 can lead to Parkinson-like symptoms, which can be cured by genetically elevating Nurr1 levels.
Researchers have long suspected that boosting Nurr1 with a drug might similarly slow or stop the progression of Parkinson's disease in humans, and the Michael J. Fox Foundation, which supports Parkinson's research, has listed it as one of its top priority therapeutic targets. But so far, more than a decade of efforts on this front have failed. Unlike other transcription factors, Nurr1 does not have the standard molecular "pocket" that pharmacologists typically look for when designing new drugs, leading some to surmise that nothing naturally binds Nurr1, rendering the molecule "undruggable."
But England and her team reasoned that for Nurr1 to be able to perform one of its key functions -- maintaining proper levels of dopamine in neurons -- the molecule must be able to sense unbalanced dopamine levels and restore homeostasis to the system based on some chemical signal. If scientists could identify this signal and replicate it with a drug, it could lead to a new "upstream" approach to boosting dopamine levels in patients with Parkinson's disease and potentially preventing the cellular damage that triggers dopamine cells to degenerate.
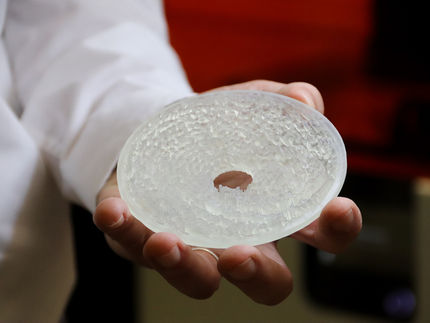
Through extensive testing, including modeling of Nurr1's structure at the atomic level, England's team showed that a molecule called DHI, a substance produced when cells dispose of excess dopamine, binds to a previously unsuspected pocket on Nurr1. Further experiments showed that adding DHI to cells in laboratory dishes and in living zebrafish boosted Nurr1 activity, stimulating genes involved in storing and producing dopamine, exactly what pharmacologists have hoped to achieve with a Nurr1-targeting drug.
While DHI itself is too unstable and reactive to be a viable drug candidate, the authors say, the discovery of how it binds to Nurr1 has produced valuable leads for scientists hoping to develop drugs to restore proper dopamine balance in Parkinson's disease, potentially slowing the progression of the disease.
"We hope these insights will lead to drugs that for the first time can target the underlying causes of Parkinson's disease," England said. "But more immediately, this discovery will allow us to better understand Nurr1's role in the earliest stages of the disease. As always, with understanding comes hope."