Test predicts outcome of hay fever therapies
Allergy researchers look into molecular processes in hyposensitization to pollen
Allergen-specific immunotherapy can make everyday life much more pleasant for allergy sufferers. It is unclear, however, what exactly happens during this treatment. A team at the Technical University of Munich (TUM) investigated the processes taking place in the body over the course of a three-year allergen-specific immunotherapy. The researchers found clues as to why the allergy immunization takes so long and how the chances of success can be determined at a very early stage.

FelixMittermeier, pixabay.com, CC0
In allergen-specific immunotherapy – once known as hyposensitization – doctors inject patients with the substances that cause allergic reactions, mostly pollen or mite allergen extracts. In the first phase of the therapy, the dose is gradually increased. Once a so-called maintenance dose is reached, the patient receives injections at that dosage over an extended period – generally three years. If all goes well, there is lasting reduction in the intensity of allergic reactions after the treatment is completed.
It is still unclear what exactly happens in the body during these treatments. A team surrounding Dr. Adam Chaker, the head of the Allergy Outpatient Clinic at the Clinic and Polyclinic for Ear, Nose and Throat Medicine at the the TUM rechts der Isar University Hospital and Professor Carsten Schmidt-Weber, head of the Center for Allergies and the Environment (ZAUM) of TUM and the Helmholtz Zentrum München, has now completed the first investigation of the complex interplay of various cell types and substances of the human immune system over the course of a three-year immunotherapy treatment.
Many different immune cells involved
In the past, allergy research has focused particularly on the role of various types of T cells.According to this – albeit highly simplified – model, pro-allergic T cells (Th2 and Th17 cells) heighten the allergic responses in the body when they encounter certain substances. Regulatory T cells (T regs), by contrast, inhibit the response to an allergen. “Our data show that the bodily processes during immunotherapy are far more complex than once believed," says Adam Chaker. "They involve cell types that have previously received very little attention in this context. In particular, we are convinced that regulatory B cells play a much more important role than we once thought.”
Test shows: the second therapy phase is not a game of chance
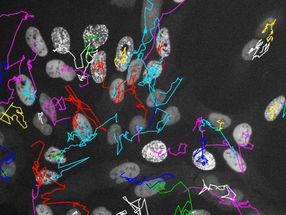
“In the second treatment phase, the body's immune system decides whether to continue launching all-out attacks on an allergen, resulting in hay fever, asthma or other allergic conditions, or whether the body will learn to tolerate the allergen,” explains Adam Chaker. The ratios of pro-allergic T cells, T regs and regulatory B-cells undergo constant change during that time. Over the course of the study, there were repeated shifts in which of the cell types was most numerous, also depending on pollen counts and other factors, with different types more prevalent at various times. It was only after around three years that the ratios gradually stabilized.
However, this phase is anything but a game of chance. In the patients who completed the treatment as planned, there were common factors that made it possible to forecast the success of the therapy at an early stage. If a lot more regulatory B-cells and a lot fewer TH-17 cells are counted immediately after the first phase, i.e. the introductory treatment phase, a significant decrease in allergy symptoms was seen after three years.
Good reasons for seeing the treatment through
“We have patented this test,” says Adam Chaker. “If we can develop it to the point where it can go into full production, we could save patients from going through expensive and time-consuming treatments with little chance of success. But in case of a positive test result, there are good reasons for seeing a three-year therapy through to the end. In the past, people have tended to give up before finishing.” In addition, a better understanding of the molecular mechanisms could serve as the basis for more effective treatments. To do that, however, it will be necessary to confirm the results of the current study through additional investigations and find out more about the mechanisms involved, says Adam Chaker.