Time-switch for immune cells
Supported by funding from the Austrian Science Fund FWF, a team from the Max F. Perutz Laboratories deciphered the mechanism of the TTP protein as a time-switch for the programmed cell death of white blood cells. A targeted death of these cells prevents an excessive immune reaction, but could also be used as a therapeutic approach for devastating tissue infections.
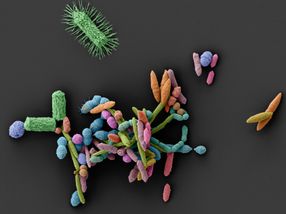
The illustration shows how the anti-inflammatory protein TTP regulates the cell death of activated neutrophils. – Perfect timing of the immune system to fight infections.
MFPL/Florian Ebner
In the case of a bacterial infection in the body, a certain type of blood cells represents the rapid reaction force of the immune system. Neutrophilic granulocytes – or neutrophils for short – are the most common white blood cells which contain potent antidotes. Because these immune cells can deliver such a strong response, they are kept in check at the site of the event by an immune regulation system, since the body’s immune response is not only about speed but also about precision and appropriate dosage. The system always tries to prevent an overshooting reaction. “It is always a tightrope walk”, stresses Pavel Kovarik: “The immune response should be strong enough to stop germs but then cut back at the right time to protect the tissue from aggressive defence mechanisms. In collaboration with a team at the Max F. Perutz Laboratories (MFPL), a research and teaching institution run jointly by the University of Vienna and the Medical University of Vienna, the immunobiologist Kovarik is investigating this fine balance in various biological processes.
Cell death timing
For the purpose of regulation, a process called programmed cell death kills off activated neutrophils after one to two days. While this process is well researched in neutrophils, the timing aspect, i.e. the mechanisms that decide when the white blood cells should die, was unclear. The MFPL team led by Kovarik discovered this temporal element by chance. Their research – supported by the Austrian Science Fund FWF – was designed to investigate the function of the anti-inflammatory protein tristetraprolin (TTP) in the regulation of the immune response against bacterial infections. To their surprise, they found that in animal experiments, where TTP had been genetically removed from neutrophils, the lifespan of the active white blood cells was extended. TTP was thus identified as a time-switch.
Life extension as a therapeutic approach
“In addition, we observed that mice without TTP in the neutrophils were better able to cope with bacterial tissue infections. We had assumed that tissue damage would become more prevalent in this group because the cell-death time-switch had become ineffective. However, prolonging the life of white blood cells seemed to have a positive effect”, explains the principal investigator, Pavel Kovarik. These findings were highly relevant because the pathogen Streptococcus pyogenes can have a devastating effect on the tissue. This frequently found bacterium usually only causes a sore throat. In a few hundred people per year in Austria, however, S. pyogenes leads to a galloping tissue infection (nectrotic fasciitis), which is often fatal.
From that moment on, the researchers focused on the conclusive elucidation of this mechanism: “We had assumed that the tissue would be damaged. The activated neutrophils also build an effective barrier that prevents germs from entering the rest of the body”, notes the immunobiologist, pointing out a potentially interesting approach for the treatment of resistant bacteria. With further test series and additional expertise from Austria and the international arena, the team was able to establish solid proof of the molecular mechanism. In mid-2017, the publication made it on to the cover of one of the oldest and most renowned biomedical journals, the Journal of Clinical Investigation, and one postdoctoral student is currently basing her application for a Marie Curie Fellowship on the results of the project.
Original publication
Florian Ebner, Vitaly Sedlyarov, Saren Tasciyan, Masa Ivin, Franz Kratochvill, Nina Gratz, Lukas Kenner, Andreas Villunger, Michael Sixt, Pavel Kovarik: The RNA-binding protein tristetraprolin schedules apoptosis of pathogen-engaged neutrophils during bacterial infection, in: Journal of Clinical Investigation, 2017
M. Ivin , A. Dumigan , F. N. de Vasconcelos , F. Ebner, M. Borroni, A. Kavirayani, K. N. Przybyszewska, R. J. Ingram, S. Lienenklaus, U. Kalinke, D. Stoiber, J. A. Bengoechea, P. Kovarik: Natural killer cell-intrinsic type I IFN signaling controls Klebsiella pneumoniae growth during lung infection, in: PLOS Pathogens, 2017