Immune system reveals new ways to treat brain disease and pain
Advertisement
Boosting the immune system could offer a radical new way to treat Alzheimer’s disease, according to Dr Michal Schwartz from the Weizmann Institute of Science in Israel. Experiments in mice have shown that targeting immune cells arrested the damage to the brain and helped preserve cognition.
For many years it was thought that there was no communication between the brain and the immune system, and that immune cells entering the brain generated pathological inflammation linked to the destruction of brain tissue seen in Alzheimer’s disease. Treatment, therefore, has targeted the immune system to suppress inflammation.
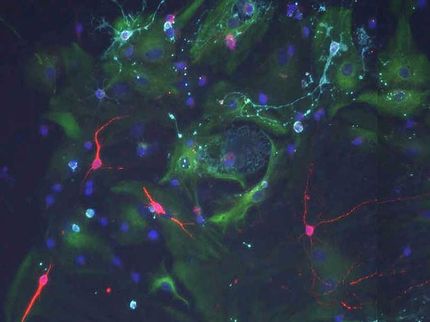
But in recent years, Professor Schwartz has accumulated evidence to demonstrate that the immune system actually protects the brain against Alzheimer’s and other neurodegenerative disorders. In particular, she discovered that the choroid plexus that produces cerebrospinal fluid acts as an interface of the so-called ‘blood-brain barrier,’ controlling the passage of immune cells in the brain. As we age, she demonstrated that the communication between the immune system and the brain is shut off.
“We turned traditional thinking on its head. We now know that inflammation - instead of causing damage - protects the brain and is essential for repairing brain tissue,” said Professor Schwartz at the FENS Forum of Neuroscience in Berlin. She carried out studies in mouse models of Alzheimer’s disease to restore the lost communication between the brain and the immune system. She found that activating the immune system drives a cascade of processes that bring in macrophages and other white blood cells that digest the damaged brain tissue.
Significantly, she found that boosting the immune activity improved memory and cognition mitigating the progress of the disease. “We gave the mice antibodies to unleash the power of the immune system. After a single injection we found that cognitive performance was improved, based on an assessment of spatial learning and memory skills. The pathology decreased and neurons were rescued,” she said.
The results indicate that directly targeting the immune system outside the brain, rather than specific factors that escalate the disease within the brain, leads to alteration of numerous processes that contribute to disease progress; this Immunotherapy may provide the first disease-modifying treatment for Alzheimer’s, as the treatment. Once the antibody has been selected and the treatment regime finalized, the next stage of her research will be a clinical trial.
A team of Harvard scientists has discovered how the bacteria that cause the flesh-eating disease, necrotising fasciitis, suppress the immune system and produce intense pain. Blocking this process with botulinum toxin is a promising strategy to treat it and some other life-threatening bacterial infections.
It is increasingly clear that nociceptors – nerves that transmit pain – and the immune system interact closely during an infection. Professor Isaac Chiu’s team at Harvard Medical School, Boston, USA have found that nociceptors, like the immune system, sense bacteria and toxins, leading to hypersensitivity and pain.
The bacteria that causes flesh-eating disease is called streptococcus (S) pyogenes. Professor Chiu told delegates at the FENS Forum of Neuroscience today (8 July), “Streptococcus pyogenes hijacks the body’s immune system to ensure its own survival. This causes pain out of all proportion to the early symptoms, and often, eventually, the death of the infected person.”
In response to the pain-inducing action of S pyogenes, the nociceptors release a chemical into infected tissues that prevents the immune system recruiting white blood cells required to fight the infection and also blocks the immune cells’ ability to release an enzyme that kills bacteria. However, Professor Chiu’s team has discovered that injections of botulinum toxin, which is used for cosmetic dermatology and treatment of migraines, can stop the bacteria causing such damage.
Experiments in mice that were injected with botulinum toxin before being exposed to S pyogenes dramatically decreased the flesh-eating ability of the bacteria and enhanced the immune system. Botulinum toxin injections after infection occurred also slowed infection and increased the recruitment of immune cells.
Currently the only treatments for necrotising fasciitis are antibiotics – which usually cannot cope with the scale of the infection – and surgery to remove the destroyed tissue. “Preventing the nociceptors from releasing their neuropeptides with botulinum toxin makes the immune system stronger and better able to kill the bacteria,” said Professor Chiu.
Professor Chiu’s research has demonstrated how the peripheral nervous system (where nociceptors are located) can direct the immune response to enable recovery, and how the immune system responds in different ways depending on the type of infection or injury. “There is a balance: some nerves drive the immune system, others suppress it. We can now begin to tease apart the molecular mechanisms and look for ways to block neuro-immune communication,” he said.
He continued, “Our results are exciting. Antibiotics do not work well to tackle lethal infections. But if we can enhance the immune system we hope to be able to develop new treatments for pain and inflammation.”