Cancer: More targeted use of immunotherapy
Doctors are increasingly fighting cancer by stimulating patients' immune systems. SNSF-supported researchers have now discovered a method for predicting the likelihood of treatment success.
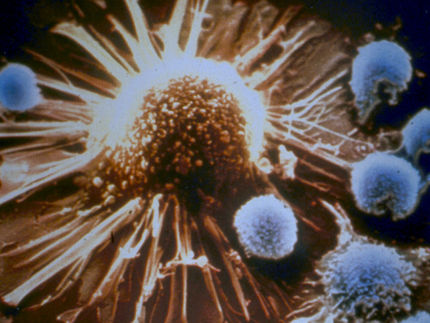
Immunotherapy changes a patient's immune system to allow it to attack cancer cells and either destroy them or at least keep them from growing. But the therapy only works for a minority of patients. Researchers supported by the Swiss National Science Foundation (SNSF) have now discovered how to better predict who will respond to the therapy and who will not.
Unmasking tumours
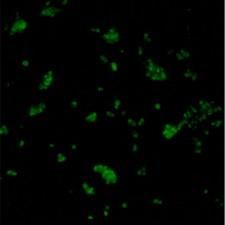
The key is a protein known as PD-1, which sits on the surface of human immune cells. Until recently, PD-1 was regarded as their Achilles heel because cancer cells attach to the protein, thereby protecting themselves from immune system attack. "It's as though the tumour were wearing camouflage", says project lead Alfred Zippelius, Deputy Head of Medical Oncology at University Hospital Basel. Immunotherapy blocks the attachment site so the immune cells can "see" the cancer again.
An international research group led by Zippelius has now shown that immune cells with the most PD-1 are best able to detect tumours (*). In addition, these PD-1–rich cells secrete a signalling compound that attracts additional immune cells to help fight the cancer. "Therefore these patients have a better chance of responding to immunotherapy", says Daniela Thommen, first author of the study, who is currently at the Netherlands Cancer Institute in Amsterdam on an SNSF mobility fellowship.
Increasing the success rate
At present, still only a fraction of patients respond to immunotherapy. "If we could tell from the outset who the therapy will work for, we could increase the success rate. That would reduce side effects and also lower costs", says Zippelius.
The new findings will enable researchers to develop a practical tool that could ultimately help doctors to decide which patients will benefit from a simple immunotherapy approach and which will require more intensive treatment – for example a combination of chemotherapy and radiation. For that to happen, researchers must first find a way of distinguishing patients based on the amount of PD-1 in their immune cells.
Immunotherapy is becoming increasingly important. "What's revolutionary about it is that some patients may remain cured after years of treatment – even in the case of tumours that have otherwise proved resistant to therapy", says Zippelius. In the meanwhile, University Hospital Basel has set up its own tumour board (a group of doctors with different specialities) for immunotherapy.
Original publication
D. S. Thommen et al.; "A transcriptionally and functionally distinct PD-1+ CD8+ T cell pool with predictive potential in non-small cell lung cancer treated with PD-1 blockade"; Nature Medicine; 2018.
Original publication
D. S. Thommen et al.; "A transcriptionally and functionally distinct PD-1+ CD8+ T cell pool with predictive potential in non-small cell lung cancer treated with PD-1 blockade"; Nature Medicine; 2018.
Organizations
Other news from the department science

Get the life science industry in your inbox
By submitting this form you agree that LUMITOS AG will send you the newsletter(s) selected above by email. Your data will not be passed on to third parties. Your data will be stored and processed in accordance with our data protection regulations. LUMITOS may contact you by email for the purpose of advertising or market and opinion surveys. You can revoke your consent at any time without giving reasons to LUMITOS AG, Ernst-Augustin-Str. 2, 12489 Berlin, Germany or by e-mail at revoke@lumitos.com with effect for the future. In addition, each email contains a link to unsubscribe from the corresponding newsletter.
Most read news
More news from our other portals
Last viewed contents
Bacterial membrane transporter helps pathogens to hide from immune system - "Our results represent a real breakthrough, since attempts to decipher the structure of a TRAP transporter had already been going on for about 20 years"

AI and 10 seconds of voice can screen for diabetes - Scientists discover voice tech as potential game changer in Type 2 diabetes detection

New sequencing technique established for low-biomass, degraded or contaminated microbiome samples
A glow stick that detects cancer?