Einstein researchers discover 2 new ways to kill TB
indings could help tame extremely drug-resistant strains
Researchers at Albert Einstein College of medicine of Yeshiva University have found two novel ways of killing the bacteria that cause tuberculosis (TB), a disease responsible for an estimated two million deaths each year. The findings, published in Nature chemical biology, could lead to a potent TB therapy that would also prevent resistant TB strains from developing.
"This approach is totally different from the way any other anti-TB drug works," says William R. Jacobs, Jr., Ph.D., the study's senior author and professor of microbiology & immunology and of genetics at Einstein, as well as a Howard Hughes Medical Institute investigator. "In the past few years, extremely drug resistant strains of TB have arisen that can't be eliminated by any drugs, so new strategies for attacking TB are urgently needed."
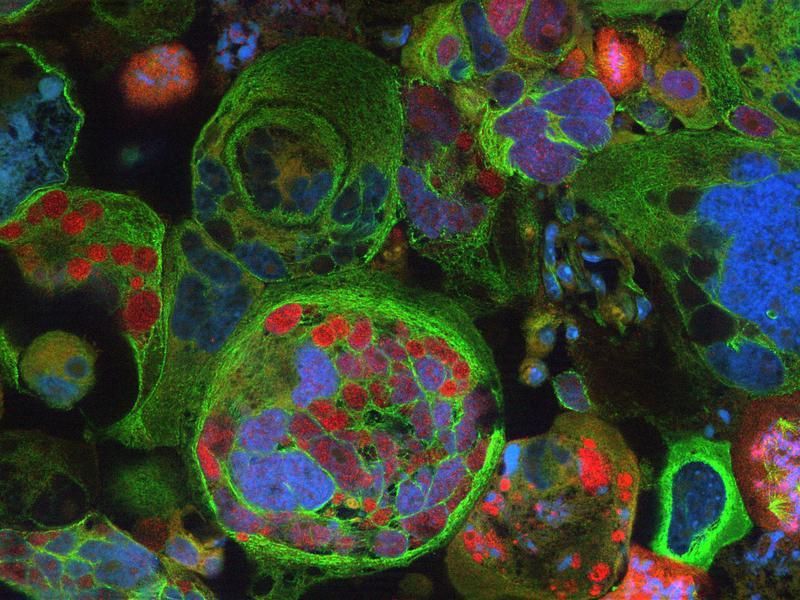
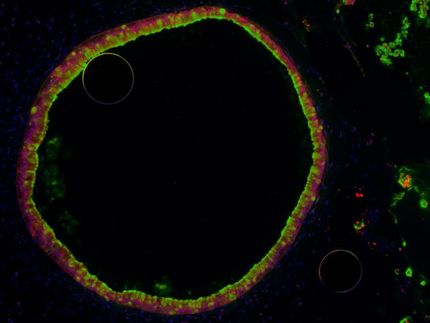
Tuberculosis is caused by the bacterial species Mycobacterium tuberculosis . In searching for a new Achilles' heel for M. tuberculosis, Dr. Jacobs and colleagues focused on an enzyme called GlgE. Previous research had suggested that GlgE might be essential for the growth of TB bacteria. GlgE would also be an excellent drug target because there are no enzymes similar to it in humans or in the bacteria of the human gut.
The GlgE research revealed a previously unknown enzymatic pathway by which TB bacteria convert the sugar trehalose (consisting of two glucose molecules) into longer sugar molecules known as alpha glucans – building blocks that are essential for maintaining bacterial structure and for making new microbes through cell division. GlgE was the third of four enzymes involved in this pathway leading to alpha glucans molecules.
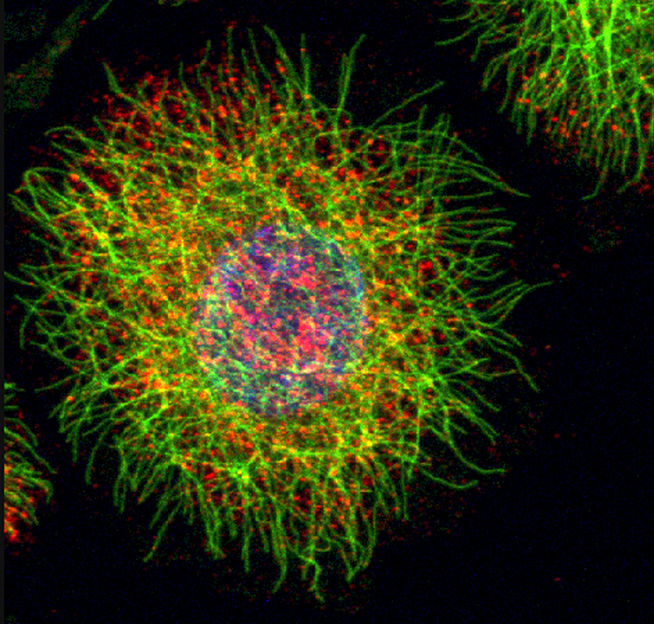
Sure enough, when the researchers inhibited GlgE, the bacteria underwent "suicidal self-poisoning": a sugar called maltose 1-phosphate accumulated to toxic levels that damaged bacterial DNA, causing the death of TB bacteria grown in Petri dishes as well as in infected mice.
"We were amazed when we knocked out GlgE that we saw this DNA damage response," says Dr. Jacobs. "That's usually a very effective way to kill bacteria, when you start damaging the DNA."
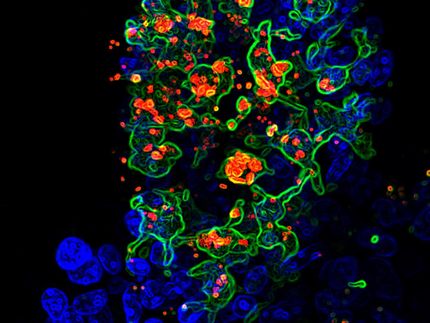
The researchers discovered a second way of killing TB after observing a crucial connection between their novel alpha glucan pathway and a second pathway that also synthesizes alpha glucans.
When the researchers knocked out one of the other enzymes in their novel pathway, the pathway's shutdown didn't kill the bacteria; similarly, inactivating an enzyme called Rv3032 in the second alpha glucan pathway failed to kill the microbes. But inactivating both of those enzymes caused what the researchers term synthetic lethality: two inactivations that separately were nonlethal but together cause bacterial death.
"The bacteria that cause TB need to synthesize alpha glucans," notes Dr. Jacobs. "And from the bacterial point of view, you can't knock out both of these alpha glucan pathways simultaneously or you're dead. So if we were to make drugs against GlgE and Rv3032, the combination would be extremely potent. And since TB bacteria need both of those alpha glucan pathways to live, it's very unlikely that this combination therapy would leave behind surviving bacteria that could develop into resistant strains."
Dr. Jacobs adds that findings from this study could also enhance treatment of diseases caused by other species of mycobacteria. Leprosy, for example, which still occurs in the U.S. and other countries, is caused by a mycobacterium related to TB. Treating leprosy now involves using several different drugs, some of which are also used to treat tuberculosis.
Original publication: "Self-Poisoning of Mycobacterium tuberculosis by targeting GlgE in an a-glucan pathway."; Nature Chemical Biology 2010.
Most read news
Other news from the department science

Get the life science industry in your inbox
By submitting this form you agree that LUMITOS AG will send you the newsletter(s) selected above by email. Your data will not be passed on to third parties. Your data will be stored and processed in accordance with our data protection regulations. LUMITOS may contact you by email for the purpose of advertising or market and opinion surveys. You can revoke your consent at any time without giving reasons to LUMITOS AG, Ernst-Augustin-Str. 2, 12489 Berlin, Germany or by e-mail at revoke@lumitos.com with effect for the future. In addition, each email contains a link to unsubscribe from the corresponding newsletter.
Most read news
More news from our other portals
Last viewed contents
Monoamine_oxidase_inhibitor
Black_Death
Protein highways keep tissues organize

Gene identified that could help prevent or delay onset of Alzheimer's disease - Boosting ABCC1 could lessen the production of plaque linked to Alzheimer's development