A golden bullet for cancer
In a lecture he delivered in 1906, the German physician Paul Ehrlich coined the term Zauberkugel, or "magic bullet," as shorthand for a highly targeted medical treatment. Magic bullets, also called silver bullets, because of the folkloric belief that only silver bullets can kill supernatural creatures, remain the goal of drug development efforts today. A team of scientists at Washington University in St. Louis is currently working on a magic bullet for cancer, a disease whose treatments are notoriously indiscriminate and nonspecific. But their bullets are gold rather than silver. Literally.

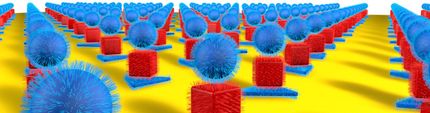
WUSTL
The gold bullets are gold nanocages that, when injected, selectively accumulate in tumors. When the tumors are later bathed in laser light, the surrounding tissue is barely warmed, but the nanocages convert light to heat, killing the malignant cells. In an article just published in the journal Small, the team describes the successful photothermal treatment of tumors in mice.
The team includes Younan Xia, Ph.D., the James M. McKelvey Professor of Biomedical Engineering in the School of Engineering and Applied Science, Michael J. Welch, Ph.D., professor of radiology and developmental biology in the School of Medicine, Jingyi Chen, Ph.D., research assistant professor of biomedical engineering and Charles Glaus, Ph.D., a postdoctoral research associate in the Department of Radiology.
Suspensions of the gold nanocages, which are roughly the same size as a virus particle, are not always yellow, as one would expect, but instead can be any color in the rainbow. They are colored by something called a surface plasmon resonance. Some of the electrons in the gold are not anchored to individual atoms but instead form a free-floating electron gas, Xia explains. Light falling on these electrons can drive them to oscillate as one. This collective oscillation, the surface plasmon, picks a particular wavelength, or color, out of the incident light, and this determines the color we see.
The resonance — and the color — can be tuned over a wide range of wavelengths by altering the thickness of the cages' walls. For biomedical applications, Xia's lab tunes the cages to 800 nanometers, a wavelength that falls in a window of tissue transparency that lies between 750 and 900 nanometers, in the near-infrared part of the spectrum. Light in this sweet spot can penetrate as deep as several inches in the body (either from the skin or the interior of the gastrointestinal tract or other organ systems). By controlling the cages' size, Xia's lab tailors them to achieve maximum absorption.
A trial run In Welch's lab, mice bearing tumors on both flanks were randomly divided into two groups. The mice in one group were injected with the PEG-coated nanocages and those in the other with buffer solution. Several days later the right tumor of each animal was exposed to a diode laser for 10 minutes.
The team employed several different noninvasive imaging techniques to follow the effects of the therapy. During irradiation, thermal images of the mice were made with an infrared camera. As is true of cells in other animals that automatically regulate their body temperature, mouse cells function optimally only if the mouse's body temperature remains between 36.5 and 37.5 degrees Celsius. At temperatures above 42 degrees Celsius the cells begin to die as the proteins whose proper functioning maintains them begin to unfold. In the nanocage-injected mice, the skin surface temperature increased rapidly from 32 degrees Celsius to 54 degrees C. In the buffer-injected mice, however, the surface temperature remained below 37 degrees Celsius.
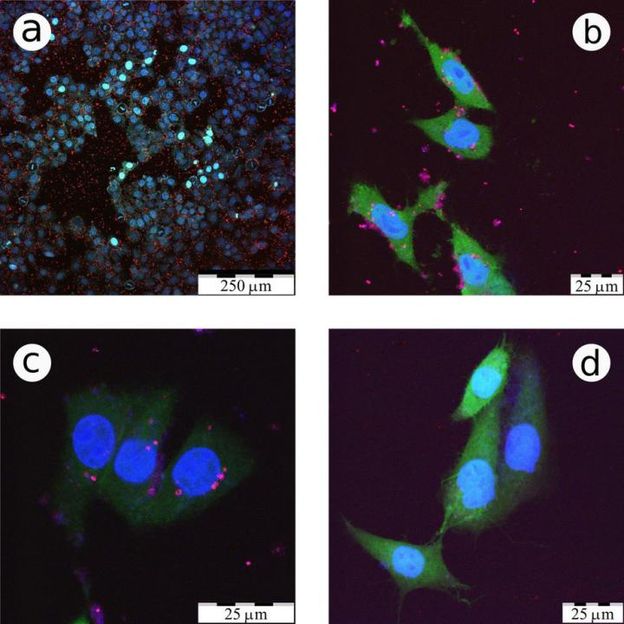
To see what effect this heating had on the tumors, the mice were injected with a radioactive tracer incorporated in a molecule similar to glucose, the main energy source in the body. Positron emission and computerized tomography (PET and CT) scans were used to record the concentration of the glucose lookalike in body tissues; the higher the glucose uptake, the greater the metabolic activity.
The tumors of nanocage-injected mice were significantly fainter on the PET scans than those of buffer-injected mice, indicating that many tumor cells were no longer functioning. The tumors in the nanocage-treated mice were later found to have marked histological signs of cellular damage.