New tool illuminates connections between stem cells and cancer
Advertisement
Researchers have a new tool to understand how cancers grow - and with it a new opportunity to identify novel cancer drugs. They've been able to break apart human prostate tissue, extract the stem cells in that tissue, and alter those cells genetically so that they spur cancer. Owen Witte, a Howard Hughes Medical Institute investigator at the University of California, Los Angeles, will present the findings at the annual meeting of the American Association for the Advancement of Science.
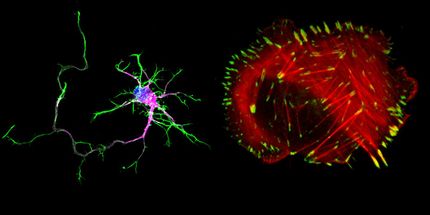
Many tissues contain pools of stem cells that replenish the tissue when it's damaged or when changes take place. For instance, stem cells in the skin produce new cells to replace those irreparably damaged by the sun, and stem cells in the breast create milk-producing cells when a woman is pregnant. The hallmark of these stem cells is that they self-renew. This means that in addition to making cells with a specific function, they also make many new stem cells.
Mounting evidence suggests that these self-renewing cells are also tied to cancer. They tend to collect mutations, says Witte, and not much separates tumor cells, with their capacity for unchecked growth, from healthy, tissue-forming stem cells. "These cells have a huge capacity for self-renewal, and when the pathways that control self-renewal are augmented or changed, they can form tumors," says Witte.
Many scientists suspect that although tumors are made up of many cells, only the tumor cells derived from stem cells contribute to the growth of the tumor. For certain cancers, such as breast cancer and leukemia, that idea is well established. For others, such as prostate cancer, which Witte studies, the data are not conclusive.
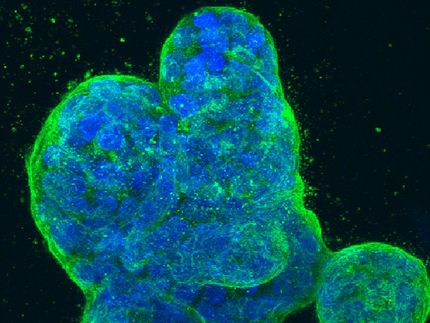
Witte's group has been analyzing the relationship between tissue stem cells and cancer stem cells in the prostate. They have been attacking this problem by dividing mouse prostate tissue into its component cell types, culturing those cells, and then reassembling them to understand how they interact. Now, for the first time, they've accomplished that feat with human tissue. Importantly, they've also engineered specific genetic changes into human prostate stem cells to transform them into cancer cells.
The group is in the early stages of putting the technique to use, but Witte says it offers some distinct advantages for developing new cancer drugs. Cells can be grown directly from a prostate tumor for use in experiments, but without knowing the precise genetics of those cells, scientists may never know why they became cancerous. Drugs that are effective in stopping their growth may not have the same impact on prostate tumors driven by different gene mutations. Starting from prostate stem cells, Witte knows exactly which genetic changes have made a cell cancerous.
"Here you can preprogram the genetic buffet, and then evaluate a compound in the face of those specific changes," says Witte.
That precision should speed the development of a new generation of fine-tuned cancer therapies. The new system should give scientists a firmer grasp of the genetic makeup of cells that are affected by particular compounds, and by extension, help clinicians identify the drugs that will best help particular patients. "The field of cancer research has produced a significant number of major new targeted therapies," says Witte. "Now we have to understand how best to use those therapies."