Newly identified genes influence insulin and glucose regulation
An international research consortium has found 13 new genetic variants that influence blood glucose regulation, insulin resistance, and the function of insulin-secreting beta cells in populations of European descent. Five of the newly discovered variants increase the risk of developing type 2 diabetes, the most common form of diabetes.
The results of two studies, conducted by the Meta-Analyses of Glucose and Insulin Related Traits Consortium (MAGIC), provide important clues about the role of beta cells in the development of type 2 diabetes. The studies, funded in part by the National Institutes of Health, appear in Nature Genetics.
"The findings from these ambitious, large-scale studies represent an enormous achievement in international cooperation involving hundreds of researchers and many thousands of individuals who contributed genetic samples for the study. The results give us exciting new directions for future research in the biology of type 2 diabetes, which poses a major and growing public health problem worldwide," said NIH Director Francis S. Collins, M.D., Ph.D., an author of both papers.
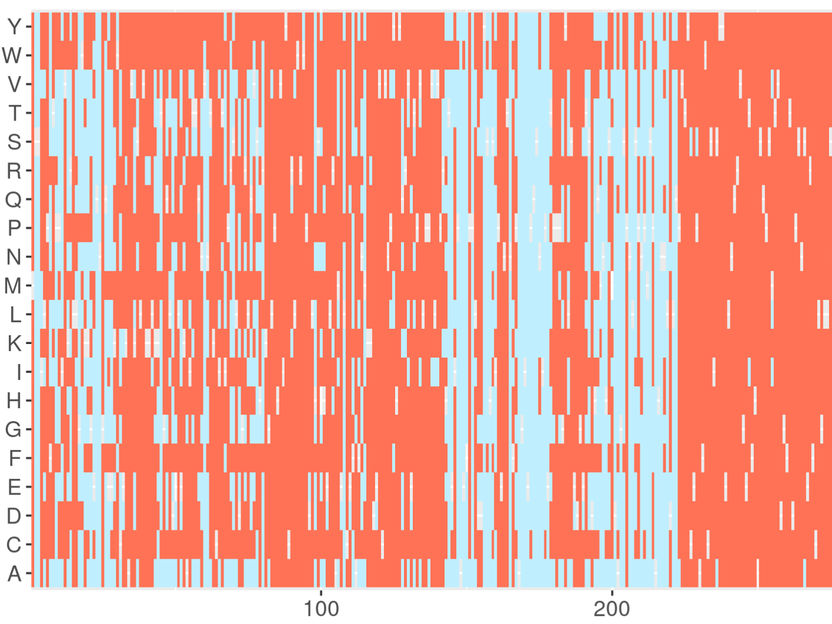
In one paper, the MAGIC investigators set out to find genes that influence metabolic traits, including fasting glucose and insulin levels and measures of beta cell function and insulin resistance. About 2.5 million genetic variants were analyzed in 21 genome-wide association studies (GWAS) that had enrolled 46,186 individuals who did not have diabetes and had been tested for measures of glucose and insulin regulation. GWAS look for common genetic associations by scanning the DNA of thousands of individuals. The huge numbers of genetic samples boosts the chances of finding subtle associations of genetic variants with specific diseases or traits. The most common variation is a change in a single nucleotide polymorphism (SNP), or single base pair change, in one of the building blocks of DNA.
The initial analysis yielded 25 candidate SNPs that were further tested in genetic samples from about 77,000 additional individuals. This step led to 16 SNPs that were clearly associated with fasting glucose and beta cell function and two SNPs associated with fasting insulin and insulin resistance. The investigators then asked whether any of the SNPs raise type 2 diabetes risk by comparing gene variants from thousands of people with and without type 2 diabetes.
Among the five variants that raise type 2 diabetes risk, one of the more intriguing SNPs is in the region of ADCY5, which influences fasting and postprandial glucose levels. Another is in FADS1, which is linked with fasting glucose as well as lipid traits. None of the variants found in the MAGIC studies were associated with type 1 diabetes, an autoimmune disease that has been traced mainly to genes that regulate immune function.
"The hallmarks of type 2 diabetes are insulin resistance and impaired beta cell function. We were intrigued to find that most of the newly found variants influence insulin secretion rather than insulin resistance. Only one variant, near IGF1, is associated with insulin resistance," said lead author Inês Barroso, Ph.D., of the Wellcome Trust Sanger Institute, Cambridge, England.
Beta cell impairment may play a larger role in type 2 diabetes than previously recognized, the authors suggest. Also, the environment may contribute to insulin resistance more than it does to insulin secretion. Learning how the genes influence cell signaling and development, glucose sensing, and hormonal regulation will assist the development of targeted methods to prevent and treat diabetes, they conclude.
Most read news
Other news from the department science

Get the life science industry in your inbox
By submitting this form you agree that LUMITOS AG will send you the newsletter(s) selected above by email. Your data will not be passed on to third parties. Your data will be stored and processed in accordance with our data protection regulations. LUMITOS may contact you by email for the purpose of advertising or market and opinion surveys. You can revoke your consent at any time without giving reasons to LUMITOS AG, Ernst-Augustin-Str. 2, 12489 Berlin, Germany or by e-mail at revoke@lumitos.com with effect for the future. In addition, each email contains a link to unsubscribe from the corresponding newsletter.
Most read news
More news from our other portals
Last viewed contents
Plant-made antibodies to control dental caries in a large scale - Large Scale Biology Corporation and Planet Biotechnology Inc. Announce Expansion of Biomanufacturing Program

Deep periodontal pockets promote dementia risk - Prevention and early treatment of periodontitis is important
New tool facilitates clinical interpretation of genetic information