Common herbal medicine may prevent acetaminophen-related liver damage, says Stanford researcher
A well-known Eastern medicine supplement may help avoid the most common cause of liver transplantation, according to a study by researchers at the Stanford University School of Medicine. The finding came as a surprise to the scientists, who used a number of advanced genetic and genomic techniques in mice to identify a molecular pathway that counters acetaminophen toxicity, which leads to liver failure.
“I didn’t know anything about the substance that was necessary for the pathway’s function, so I had to look it up,” said Gary Peltz, MD, PhD, professor of anesthesiology. “My postdoctoral fellow, whose parents and other family members in Asia were taking this compound in their supplements, started laughing. He recognized it immediately.”
The molecule was S-methylmethionine, which had been marketed as an herbal medicine known as Vitamin U for treatment of the digestive system. It is highly abundant in many plants, including cabbage and wheat, and is routinely ingested by people. Coincidentally, Garnett Cheney, MD, at Stanford University performed a series of studies in the 1950s in which he used the compound to treat peptic ulcers.
Peltz is the senior author of the research, which is published in Genome Research. The experiments were conducted in Peltz’s laboratory at Roche Palo Alto in Palo Alto, Calif., where Peltz worked before coming to Stanford in July 2008. He is continuing the research at Stanford. The first author of the paper, Hong-Hsing Liu, MD, PhD, is now a postdoctoral scholar in Peltz’s Stanford lab.
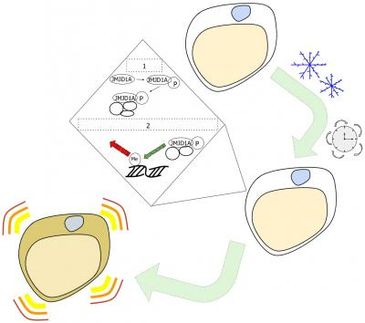
Acetaminophen is a pain reliever present in many over-the-counter cold and flu medicines. It is broken down, or metabolized, in the body into byproducts — one of which can be very toxic to the liver. At normal, therapeutic levels, this byproduct is easily deactivated when it binds to a naturally occurring, protective molecule called glutathione. But the body’s glutathione stores are finite, and are quickly depleted when the recommended doses of acetaminophen are exceeded.
Unfortunately, the prevalence of acetaminophen makes it easy to accidentally exceed the recommended levels, which can occur by dosing more frequently than indicated or by combining two or more acetaminophen-containing products. However, severe liver damage can occur at even two to three times the recommended dose (the maximum adult dose is 4 grams per day; toxic daily levels range from 7 to 10 grams).
“It’s a huge public health problem,” said Peltz. “It’s particularly difficult for parents, who may not realize that acetaminophen is in so many pediatric medicines.” Acetaminophen overdose is the most common cause of liver transplantation in this country. The only effective antidote is an unpalatable compound called NAC that can induce nausea and vomiting, and must be administered as soon as possible after the overdose.
Peltz and his colleagues used 16 inbred strains of laboratory mice for their investigations. Most strains are susceptible to acetaminophen toxicity, but one is resistant. They compared how the drug is metabolized by the different strains and looked for variations in gene expression and changes in endogenous metabolites in response to acetaminophen administration. They identified 224 candidate genes that might explain the resistant strain’s ability to ward off liver damage, and then plumbed computer databases to identify those involved in metabolizing acetaminophen’s dangerous byproducts.
One, an enzyme called Bhmt2, fit the bill: It helped generate more glutathione, and its sequence varied between the resistant and non-resistant strains of mice. Bhmt2 works by converting the diet-derived molecule S-methylmethionine, or SMM, into methionine, which is subsequently converted in a series of steps into glutathione. The researchers confirmed the importance of the pathway by showing that SMM conferred protection against acetaminophen-induced liver toxicity only in strains of mice in which the Bhmt2 pathway was functional.
“By administering SMM, which is found in every flowering plant and vegetable, we were able to prevent a lot of the drug’s toxic effect,” said Peltz. He and his colleagues are now working to set up clinical trials at Stanford to see whether it will have a similar effect in humans. In the meantime, though, he cautions against assuming that dosing oneself with SMM will protect against acetaminophen overdose.
“There are many pathways involved in the metabolism of this drug, and individuals’ genetic backgrounds are tremendously variable. This is just one piece of the puzzle; we don’t have the full answer,” he said. However, if subsequent studies are promising, Peltz envisions possibly a co-formulated drug containing both acetaminophen and SMM or using SMM as a routine dietary supplement.