Stanford study identifies cellular mechanism that causes lupuslike symptoms in mice
macrophages, the scavenger cells of the body's immune system, are responsible for disposing of dying cells. Stanford University School of medicine researchers have identified one pathway in this important process in mice that, if disrupted, causes a lupuslike autoimmune disease. The findings could lead to both a better understanding of the cause of lupus in humans and potential drug treatments for the disorder.
"Just like in mice, in humans, if you don't clear the dying cells, then that predisposes you to lupus," said Lata Mukundan, PhD, a Stanford research associate and one of the first authors of the study to be published in Nature Medicine. "If you look at patients with lupus, they have an inability to clear those dead cells."
Added Ajay Chawla, MD, PhD, assistant professor of endocrinology and senior author of the study: "The clearing away of dying cells is important. If they're not cleared away, they can provide antigens against ourselves, leading to development of autoimmunity."
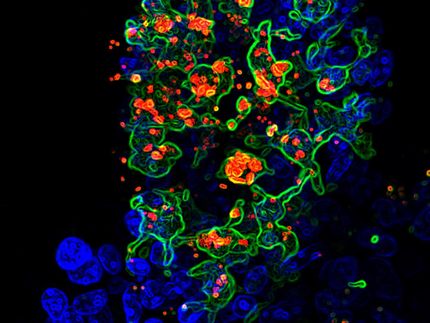
Mukundan, Chawla and their colleagues have uncovered one of the pathways by which macrophages sense and silently dispose of these dying cells — a naturally-occurring process not previously understood — by conducting lab experiments in vitro with mouse and human macrophages, as well as in genetically engineered mice. Researchers hypothesized that a molecule in the nucleus of cells called PPAR-delta plays a pivotal role in orchestrating the timely disposal of dying cells by macrophages, the white blood cells that swallow and digest cellular debris and pathogens, triggering other immune cells to aid in the response to a pathogen.
"We wanted to know, if you took a mouse and only deleted PPAR-delta from its macrophages, is that sufficient to cause an autoimmune disease?" Chawla said. "Apparently it is."
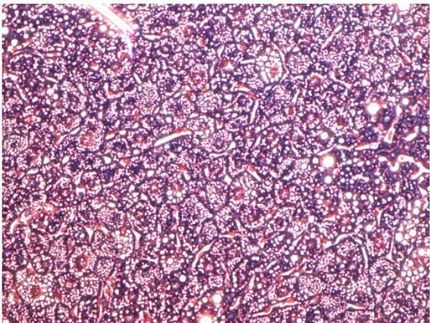
To test their theory, researchers bred genetically engineered mice that were missing the PPAR-delta molecule in their macrophages, and then injected them with apoptotic (dying) cells. It turned out that simply missing the PPAR-delta molecule caused a lupuslike autoimmune kidney disorder in mice. Drugs that activate PPAR-delta have been identified and are in clinical trials for treatment of high blood cholesterol and other lipid disorders. Thus, the direct involvement of PPAR-delta in suppressing autoantibody production and maintaining the body's tolerance to itself raises the possibility that these molecules that activate PPAR-delta can be used to treat patients with lupus.
The study pinpoints how PPAR-delta works in macrophages. When the macrophages eat dying cells, certain genes get turned on in these cells, triggering further consumption of more dying cells and aiding in their clearance.
First, PPAR-delta aids in the recognition of the dying cell by regulating the production of key proteins called opsonins. These proteins recognize the "eat me" signals released by the dying cells. In addition, PPAR-delta also prevents the immune system from mounting an inflammatory response to the dying cell and thus functions in the safe disposal of the dying cells. In the absence of PPAR-delta, mice have an accumulation of dead cells that over time delivers a danger signal to the immune system, leading to inflammation and tissue damage.
"The dying cells are a bunch of modified lipids," Chawla noted.
When the macrophages eat the dying cells it doubles their content of lipids. The team showed in additional experiments in the lab that the lipids worked as a signal to tell the macrophages they needed to eat more dying cells. "These receptors allow the macrophages to turn on the genes for better clearing in the body," Chawla said.
Most read news
Topics
Organizations
Other news from the department science

Get the life science industry in your inbox
By submitting this form you agree that LUMITOS AG will send you the newsletter(s) selected above by email. Your data will not be passed on to third parties. Your data will be stored and processed in accordance with our data protection regulations. LUMITOS may contact you by email for the purpose of advertising or market and opinion surveys. You can revoke your consent at any time without giving reasons to LUMITOS AG, Ernst-Augustin-Str. 2, 12489 Berlin, Germany or by e-mail at revoke@lumitos.com with effect for the future. In addition, each email contains a link to unsubscribe from the corresponding newsletter.